Chapter 5
Testing Cognitive Function at the Bedside
Introduction
The general schema followed is that already outlined in Chapters 1 and 3. The first part of the examination should assess distributed cognitive functions; deficits in these indicate damage to particular brain systems, but not to focal areas of one hemisphere. The second part of the assessment should deal with more localized functions, divided into those associated with the dominant (i.e. the left side, in right-handers) and non-dominant hemispheres.
The Addenbrooke’s Cognitive Examination (ACE), which has now been revised (ACE-III), is described in Chapter 7. The ACE-III takes approximately 15 minutes to complete and can be regarded as a basic screening instrument that is particularly useful in an outpatient setting. It was developed principally to aid in the detection and monitoring of dementia syndromes and is less valuable in the diagnosis of delirium or other cognitive disorders. Specific shortcomings and pitfalls are discussed in the following sections, and in the context of the illustrative cases in Chapter 8.
Cognitive assessment should always follow history taking, because invaluable information is gained from the patient and informant, which guides the examination. For instance, even minor degrees of aphasia should be apparent from history taking, and will lead the examiner to assess language function thoroughly.
General Observations
Mood and motivation are essential to all mental functions. The degree of cooperation, the ability to sustain effort, and the amount of encouragement required to complete a task are all observable aspects of motivation. A disturbance in motivation is described as ‘apathy’, and if it is extreme the term ‘abulia’ is used.
Behaviour during the examination should be noted. Does the patient interact appropriately? Frontally damaged patients are often inappropriately jocular, or make puerile or obscene comments. Patients with acute confusional states (delirium) show either increased or decreased psychomotor activity. In the former state, patients are restless, voluble, noisy, fidgety, and distractable. In the latter, hypo-alert variant of delirium, patients are quiet, speak little, and drift easily off to sleep if unstimulated.
Orientation and Attention
The examination should begin by testing the patient’s orientation and attention abilities (see Table 5.1).
Table 5.1 Summary of bedside testing for orientation and attention
| Alertness | Level of wakefulness and reactivity | |
|---|---|---|
| Orientation |
Time |
Day of week |
| Date | ||
| Month | ||
| Season | ||
| Year | ||
|
Place |
Building | |
| Floor | ||
| Town | ||
| County | ||
| Country | ||
| Attention/concentration |
Serial subtraction of 7s |
|
|
Months of year backwards |
||
|
Days of week backwards |
||
|
Digit span forwards and backwards |
||
|
Formal tests: stroop test, Speeded letter cancellation tasks, Trails A, and the Test of Everyday Attention (TEA) which consists of a number of subtests designed to assess subcomponents of attention. The PASAT test and components of the CANTAB battery (see Appendix) |
||
Alertness
Record the level of wakefulness of the patient. It is hopeless to attempt a detailed cognitive assessment in a drowsy patient. A common-sense description such as ‘awake and fully cooperative’ or ‘cooperative but sleepy, with a tendency to doze off if unstimulated’, is much better than vague, undefined terms such as ‘obtunded’ or ‘stuporose’.
Orientation
This is conventionally divided into time and place. Of these, the first is the most important and clinically helpful.
Time
Time orientation should always include the day of the week, date, month, season, and the year. Date orientation is the least reliable, since some normal subjects do not know the exact date. When assessing inpatients, the question ‘How long have you been in hospital?’ is often helpful. Even mildly delirious patients frequently over- or under-estimate the passage of time, thinking that they have been in hospital for days when, in fact, they were admitted only that morning.
Disorientation in time is common in patients with acute confusional states (delirium) due to metabolic disorders or diffuse brain injury. It is also seen in patients with moderate-to-severe (but not mild) dementia, due to a combination of amnesia and attentional deficits, and in the amnesic syndrome.
Note: many patients with clinically significant memory impairment remain well orientated in time. Orientation in time should not, therefore, be taken to exclude a significant memory disorder.
Place
I usually use a question along the lines of ‘What is the name of this building?’. It is surprising how often patients are unaware that they are in hospital, a fact that is easily overlooked if the examiner simply asks for the name of the hospital. Orientation in place is less sensitive than time orientation to attentional and memory deficits. The Mini-Mental State Examination (MMSE) and the ACE- III include orientation for town, county, and country but these can usually be omitted in bright, alert, and other well-oriented patients.
It is rare for patients to be unable to tell you their names. Even very confused or demented subjects do not show this deficit. But it is a characteristic feature of psychogenic (hysterical) amnesia. Aphasic patients may also be unable to access their own names, but when given a choice, such as ‘Is your name Frank, John, or Harry?’, can usually pick out the correct name. Patients with aphasia are frequently misdiagnosed as confused because they are unable either to comprehend the question or to produce the correct answer. This error should be avoided if the patient is engaged in casual conversation before plunging into formal cognitive assessment. Also included as part of person orientation are age and date of birth.
Attention/concentration
Ability to sustain attention and keep track of ongoing events can be assessed in a number of ways, including digit span, serial subtraction of 7s, spelling of familiar words backwards (for instance, WORLD—DLROW), and recitation of the days of the week or the months of the year in reverse order. The two alternatives in the MMSE (serial 7s and WORLD backwards) are problematic. Many normal elderly subjects make errors of serial subtraction, as do patients with focal left hemisphere damage and the scoring of omissions, substitutions, and reversals is complicated. In the MMSE and ACE-III, subjects are asked to spell WORLD backwards if they make any errors on the serial subtraction task. The scoring system is explained in Chapter 7. Recitation of the months of the year is an over-learnt sequence, familiar to everyone. The ability to recite these in reverse order is therefore a good measure of sustained attention. Patients should be fast and errorless at this simple test. If the patient is unable to do this, try the days of the week backwards instead.
Digit span
Digit span, especially reverse digit span, is a more accurate measure of attentional processes, and a useful adjunct to the mentioned measures. The ability to repeat a string of digits has little, if anything, to do with the processes involved in laying down and retrieving new episodic (event) memories. Digit repetition depends upon short-term (working) memory, which in turn depends upon frontal executive and phonological processes (see ‘Short-term (working) memory’ in the ‘Memory’ section in Chapter 1). Reduction in digit span is a feature of impaired attention, as found in acute confusional states or moderate-to-severe dementia, and may also occur in patients with focal left hemisphere lesions. Patients with aphasia typically have a reduced digit span.
Note: patients with the amnesic syndrome (for example, Korsakoff’s disease or early Alzheimer’s disease), who may be totally unable to lay down any new episodic memories, have a normal digit span.
Digit span is tested by asking the patient to repeat a progressively lengthening string of digits. It is usual to start with three digits. Two trials are given at any level. If subjects pass on the first or on the second trial, then the next-length sequence is administered. Digit span is the highest level at which the patient passes either trial (see Box 5.1). The number should be read by the examiner at a rate of one per second—without clustering, which aids repetition: you only have to think of the usual way in which we recall telephone numbers.
| Box 5.1 Forward digit span: example |
|
6–2–7 correct 8–3–6 not administered 1–7–4–9 incorrect 7–2–5–1 correct 4–9–3–1–6 incorrect 3–8–4–7–9 incorrect Forward span = 4 (impaired) |
Exactly the same technique is employed on reverse digit span; however, here the patient is required to repeat the numbers in reverse order. It may be necessary to give some patients several demonstrations at two digits. Normal digit span is 6 ± 1, depending upon age and general intellectual abilities. Thus an intelligent young adult would be expected to have a forward span of at least 6. In the elderly, or those of low intellectual ability, 5 can be considered normal. Reverse span is usually one less than forward span (see ‘Short-term (working) memory’ in the ‘Memory’ section in Chapter 1 for further details). Digit span was not included in the ACE-III since it is quite time-consuming and prone to produce erroneous results if numbers are clustered.
Episodic Memory
As has been previously discussed in greater detail (see Chapter 1), there are many subcomponents to memory. To recap: in psychology, short-term memory applies to the system of working memory responsible for the immediate recall of small amounts of verbal or spatial information (tested at the bedside by digit span or immediate recall of a name and address), which bears little relationship to other aspects of clinically important memory. What we normally think of as memory—the capacity to learn and recall personally experienced events such as a meeting yesterday or last year’s holiday—comes under the heading of episodic memory.
In clinical terms, episodic memory function is best considered as anterograde (i.e. the ability to learn new information) and retrograde (i.e. the recall of old information) (see Table 5.2). This distinction is particularly useful since different pathological processes may differentially affect one or other of these components. Semantic memory describes our permanent store of knowledge about things in the world, as well as about words and their meanings.
Table 5.2 Episodic memory function
| Anterograde verbal |
Incidental recall of earlier conversation, journey to hospital, events on ward, etc. Recall of three items from MMSE Name and address learning, recall and recognition in ACE-III Formal tests: story recall (logical memory); word-list learning tests (Rey Auditory Verbal Learning test; California Verbal Learning Test, etc.); parts of the Doors and People Test; paired associate learning and other components of the Wechsler Memory Scale |
| Anterograde non-verbal |
Recall of shapes Formal tests: Rey–Osterrieth Complex Figure Test; Recognition Memory Test (faces); pattern–spatial associative paired learning test or PAL from the CANTAB computerized battery |
| Retrograde |
Famous events, for example: Remote personal (autobiographical) memory: Autobiographical Memory interview (AMI) |
Anterograde verbal memory
An informal, but often very revealing, impression of memory can be gained by asking patients to recall the details of very recent events, such as their journey to hospital, what they watched on TV last weekend, or a recent holiday. As a naturalistic test of episodic memory, I frequently employ the following technique: at the beginning of the interview, in the course of our general conversation, I find a topic of interest, such as the patient’s family or a recent holiday, and tell the patient something about my own interests, family, or holiday. Then later I ask the patient to recall these facts.
Name and address recall
As part of the ACE-III we ask the patient to repeat a simple seven-part name and address. This is repeated three times, even if entirely correct on the first or second trial, to ensure that it has been attended to and processed. Since repetition is within the span of short-term (working) memory, this is a measure of general attentional processes rather than of memory proper. After approximately 10 minutes (the actual time is not critical), after completing the rest of the ACE-III, the patient is asked to recall the name and address. It should be noted that this is a relatively crude measure. Total failure, or recall of one or two elements, is clearly abnormal at any age. Completely correct recall shows that the patient does not have a major amnesic deficit, although some patients shown to have a significant memory deficit on formal testing score perfectly on this simple task. Intermediate results are always more difficult to interpret. The ACE-III also contains a recognition component which is administered for those elements that patients have failed to recall. Patients with true amnesia typically fail on the recall and recognition components or improve only slightly when given a choice, ‘Was it Kingsbridge, Dartington, or Exeter?’, whereas patients with anxiety, depression, and frontal retrieval-based memory problems typically improve markedly. Thus the discrepancy between recall and recognition can be clinically very helpful. Clinical intuition is important. If informants are concerned about a patient’s memory, even if the defect is not obvious on simple testing, then formal neuropsychological evaluation is required.
Formal assessment
For those interested, and who do not have access to professional neuropsychological assessment, I would recommend two measures: story recall (logical memory) and word-list learning. Both are quick and relatively foolproof. Furthermore, there are good normative data to guide interpretation. Several versions of stories for recall exist, all of which derive originally from the Wechsler Memory Scale. There are numerous word-list learning tasks. One of the most widely used is the 15-item Rey Auditory Verbal Learning Test (RAVLT) which consists of five learning trials, of list A, then an ‘interfering’ list B followed by recall of A again, and finally, after 20 minutes, a delayed recall of list A and a yes–no recognition phase. Another commonly used test in Memory Clinics is the Grober–Buschke Selective Reminding Test. Examples of these tests are given in the Appendix. For a more thorough evaluation of memory abilities, the Wechsler Memory Scale-III, the Rivermead Behavioural Memory Test (RBMT), or the Doors and People Test are excellent all-round memory assessment instruments.
Anterograde non-verbal memory
In the vast majority of patients with memory disorders, non-verbal memory parallels verbal memory. Damage to the non-dominant—usually right—medial temporal lobe structures may, however, cause a selective non-verbal memory problem, such as a difficulty with learning faces, geometrical figures, or routes. Patients with early Alzheimer’s disease are also typically impaired on tests of non-verbal memory such as the Paired Associate Learning (PAL) test from the computerized CANTAB battery. Unfortunately there is no easily administered bedside test of non-verbal memory. Spatial learning can be tested by walking a route around the ward or clinic with the patient, and then asking him or her to repeat this route alone. Ad hoc tests of face memory can be made using photographs from magazines of non-famous faces. The Rey–Osterrieth Complex Figure Test provides very good information on non-verbal memory. The subject is first asked to copy the figure (which is obviously a test of visuospatial skills), and then, after a delay of 30–45 minutes, without being forewarned, the subject is asked to reproduce the figure from memory. Normative data are available.
The Recognition Memory Test is a valuable standardized test of verbal and non-verbal recognition memory. In the face memory subtest, subjects are shown 50 faces, each for 3 seconds, and asked to make a value judgement as to whether they find the face pleasant or not. After finishing this part of the test, they are then given 50 pairs of faces, each containing one of the previously encountered faces, and asked to say which they have seen before. Normal subjects perform surprisingly well on this test, and good normative data are available. The Rivermead Behavioural Memory Test also contains subtests that assess picture (object) recognition and recall of a route around the room (see Appendix).
Retrograde memory
Assessment of retrograde or remote memory is impressionistic at best, but a reasonable overall picture can be achieved by systematic questioning about a range of past events from the preceding months, years, and decades. Interpretation must be tempered by the patient’s probable baseline performance. For instance, elderly women are unlikely to know in detail about recent sporting events, and many normal subjects’ grasp of political events is extremely sketchy! Recall is harder than recognition, so start with open questions, such as ‘Can you tell me about any recent news items?’ or ‘What important events have been in the news lately?’. Amnesic patients often have a rough idea, so it is important to probe for specific details. It is useful to ask about a standard list of famous events, examples of which are given in Table 5.2. In many patients with retrograde memory impairment, there is a temporal gradient. That is to say, they are much better at more distant events, and become progressively more impaired the nearer you get to the present. Patients with diencephalic amnesia (for example, Korsakoff’s syndrome) and Alzheimer’s disease have a very extensive remote memory impairment. In pure hippocampal damage the retrograde loss may be more limited—a year or two at most although this is a controversial topic (see ‘The amnesic syndrome: cognitive neuropsychology’ in the ‘Memory’ section in Chapter 1).
The other domain of remote memory is personal or autobiographical memory. An impression of the patient’s capacity in this area is best formed during history taking. Can the patient accurately relate, and in the correct chronological sequence, events and details of his or her own life? The best formal test of remote personal memory is the Autobiographical Memory Interview (see Appendix).
Semantic Memory
Since semantic memory underlies so many aspects of cognition—our ability to produce and understand words, interpret pictures, recognize faces, and so on— there is no single test of semantic memory. Deficits are typically detected using verbal tasks but are also present when patients are tested using non-verbally based tasks (see Box 5.2).
Category fluency is a very sensitive task but is also affected by other factors such as executive function. The interpretation of verbal fluency tests is discussed later in this section (see also ‘Executive abilities’ in the ‘Higher-Order Cognitive Function, Personality, and Behaviour’ section in Chapter 1).
Confrontation naming also detects semantic deficits with the production of broad subordinate responses (e.g. ANIMAL for RHINOCEROS, or MUSICAL THING for HARP). To confirm that the anomia is not due to a perceptual deficit, or simply due to word-finding problems, it is important to check that visual processing is intact and to probe knowledge in other ways. The former can be done easily by asking the patient to describe the unnamed pictures or to copy the drawings. Patients with semantic dementia can typically identify that something is an animal but have no idea about what kind of animal it is. They can also copy the line drawings and match together two drawings of the same thing. The fact that their problem reflects breakdown in underlying semantic knowledge is confirmed by word definition tests. If unable to name a picture of a rhinoceros, they typically can produce only very limited information in response to the name ‘rhinoceros’.
| Box 5.2 Tests for semantic memory functions |
|
Category fluency (generation of exemplars from categories such as animals, fruit, etc.). Naming pictures. Tests of verbal knowledge (generation of definitions from words or pictures). Picture pointing in response to the spoken name. Non-verbal tests such as the Pyramids and Palm Trees Test or the Camel and Cactus Test from the Cambridge Semantic Memory Battery. Person knowledge tests. |
The ability to point to a correct target in response to the command ‘point to the rhinoceros’ is critically affected by the foils. That is to say, it is much easier if all the other possible choices are non-animals and hardest if they are other foreign animals. Tests using non-verbal materials such as the Pyramids and Palm Trees Test of associative knowledge are required to confirm the presence of a semantic memory deficit but these are beyond the realm of bedside testing.
Most patients with semantic deficits are particularly poor at naming and identifying famous faces but those with right temporal lobe damage show selective and often profound difficulties in this domain.
Frontal Executive Functions
The history obtained from an informant and general clinical observations of the patient’s behaviour are more important than formal bedside testing for the overall assessment of the higher-order or executive functions. However, there are a number of measures which can be helpful in confirming clinical impressions (see Table 5.3).
Initiation: verbal fluency tests
The generation of words beginning with a specified letter, or from a common semantic category (for example, animals, fruit, etc.) depends on the coordinated activity of two main cerebral areas—the frontal lobes (which generate retrieval strategies) and the temporal lobes (where semantic knowledge is stored). Therefore, in the absence of a semantic deficit or aphasia, verbal fluency is a good test of frontal lobe function. In the standard version of the letter fluency test, patients are asked to generate as many words as possible, excluding names of people or places, in 1 minute. The most commonly used letters are F, A, and S. Normal young subjects should produce at least 15 words for each letter. A total for FAS of less than 30 words is abnormal; but some allowance should be made for age and background intellect. In the ACE-III we use the letter ‘P’ and calculate a scaled score of 0–7 depending on the number of novel correct words produced (see Chapter 7).
Table 5.3 Tests for the assessment of frontal executive functions
| Initiation |
Verbal fluency tests: |
| Abstraction |
Proverb interpretation, e.g.: Similarities test, e.g.: |
|
Formal test: Cognitive Estimates Test (see Appendix) |
|
| Problem-solving and decision-making |
Formal tests: Tower of London Test (see D-KEFS test) or the Stocking of Cambridge version in the CANTAB battery and The Iowa or Cambridge Gambling Test from the CANTAB battery |
| Response inhibition |
Alternating sequences |
| and set shifting |
Go–No-Go Test |
|
Motor sequencing tests (Luria Three-Step and Alternating Hand Movements) |
|
|
Formal tests: Wisconsin Card Sorting Test (WCST) and Trail Making Test: Part B (see Appendix). The CANTAB battery includes a test similar to the WCST, the ID-ED shift test, as well as other tests of working memory and mental flexibility. The Stroop Test. The Behavioural Assessment of the Dysexecutive Syndrome (BADS) consists of more ecologically based tasks such as the six elements, zoo map, and key search subtests. The Hayling and Brixton tests are also useful recent tests of response inhibition and anticipation. |
In category fluency tasks, subjects are asked to generate as many examplars as possible from semantic categories such as animals, fruit, and vegetables. For the category animals (used in the ACE-III), normal subjects produce around 20 items in a minute; 15 is a low average, and 10 is definitely impaired. Performance drops with age, and for the very elderly 10 may be just about acceptable. A reversal of the usual pattern (animals better than letter ‘P’) is highly suggestive of a semantic memory deficit.
As well as absolute numbers on both tasks, a note should be made of the number of perseverative responses. Normals do not perseverate. Patients with severe amnesia may produce perseverative errors; but in general they are a feature of frontal lobe disease or dysfunction of frontal lobe connections (for example, Huntington’s and Parkinson’s diseases).
A related and clinically useful task is the Supermarket Fluency Test: subjects are asked to list all the things that can be bought in a supermarket. Normal subjects systematically search various subcategories (dairy produce, fresh fruit, etc.), giving a few examples of each. On this test around 20 items is average, 15 is poor, and below 10 is definitely impaired. Patients with frontal dysfunction show poor organization strategies and perseverative responses. In Alzheimer’s disease, the patients attempt to search various categories, but produce few exemplars.
Abstraction: proverbs, similarities, and cognitive estimates
Some impression of abstract conceptualization can be gained from proverb interpretation and the similarities test. Suggestions of proverbs for administration are given in Table 5.3. Concrete interpretation, with an inability to make analogies, characterizes the performance of patients with frontal lobe damage: for instance, ‘too many cooks spoil the broth’ is typically interpreted by such patients as referring to the cooking and making soup rather than its more general or abstract meaning. Interpretation of proverbs is, however, dependent upon educational level and cultural background so the results need to be interpreted with caution.
The similarities test involves asking subjects in what way two conceptually linked items are alike, starting with simple pairs such as ‘apple and banana’ and ‘table and chair’, and progressing to more abstract pairs such as ‘poem and statue’ and ‘praise and punishment’. The normal response is to form an abstract category (for example fruit, furniture, works of art). Patients with frontal deficits and dementia make very concrete interpretations (for example, table and chair: ‘you sit at one to eat from the other’ or ‘both have legs’) and often continue to do so despite being asked to think of other ways in which the items are alike. Another useful test of conceptualization is the Cognitive Estimates Test, in which patients are asked a range of questions that require common-sense judgement to answer. Examples are ‘How fast do horses gallop?’, ‘What is the height of the London BT Tower?’, ‘What is the height of an average Englishwoman?’ and ‘How many camels are there in Holland?’. Frontal patients give bizarre and illogical answers to these questions. The full test is given in the Appendix.
Response inhibition and set shifting
The ability to shift from one cognitive set to another, and to inhibit inappropriate responses, cannot be easily tested at the bedside.
Wisconsin Card Sorting Test
The best formal test of set shifting is the Wisconsin Card Sorting Test (WCST), which also involves problem-solving and hypothesis testing. The subject has to sort cards containing geometric forms which differ in number, shape, and colour. Having deduced the correct sorting dimension, the subject is then required to shift to another dimension (for example, from colour to shape) on a number of occasions. Patients with frontal lesions are unable to shift from one sorting criterion to another, and make perseverative errors. The Appendix contains a fuller description.
Alternating Sequences Test
This test is insensitive except in patients with gross deficits. The examiner produces a short sequence of alternating square and triangular shapes (see Fig. 5.1). The patient is asked to copy the sequence, and then to continue the same pattern until the end of the page. Patients with frontal lobe deficits may repeat one of the shapes rather than continuing to alternate the pair.
Go–No-Go Test
Response inhibition can be tested using this paradigm. The patient is asked to place a hand on the table and to raise one finger in response to a single tap, while holding still in response to two taps. The examiner taps on the undersurface of the table to avoid giving visual cues. Patients with frontal deficits cannot inhibit raising one finger in response to the ‘no-go’ signal. Again, this is a relatively insensitive test, so that any abnormality is highly pathological.
Trail Making Test
This is a good quantitative measure of mental speed, attention shifting, and response inhibition. On Part A, the patient must draw a line connecting randomly arranged numbers in numerical sequence (1–2–3, and so on). On Part B, the numbers are intermixed with letters, and the test is to draw a line connecting numbers and letters in an alternating sequence so that the connecting line goes from 1 to A to 2 to B to 3, and so on. Performance is influenced by intelligence and age. Age norms are available. An example of the test and normative data are given in the Appendix.
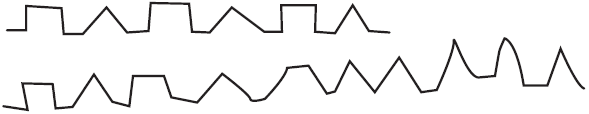
Fig. 5.1 An example of a frontal patient’s copy of an alternating sequence.
Motor Sequencing: The Luria Three-Step Test and the Alternating Hand Movements Test
Deficits in sequencing complex motor movements are associated particularly with left frontal lesions. A number of tasks can be used, of which the ‘Luria Three-Step’ and Alternating Hand Movements Tests are most helpful. In the former, the examiner demonstrates the series of hand movements—fist, edge, palm—five times without verbal clues, and then asks the subject to repeat the sequence. Patients with frontal deficits are unable to reproduce the movements, even if given specific verbal clues.
In the Alternating Hand Movements Test, the examiner again demonstrates the movement. The examiner starts with arms outstretched, one hand with fingers extended and the other with clenched fist. Then the hand positions are reversed by alternately opening and closing each hand in a rhythmical sequence.
Dominant (Left) Hemisphere Functions
The second part of the bedside cognitive assessment should address more localized functions associated with the dominant and non-dominant hemispheres. Functions associated with the left hemisphere, which is nearly always dominant for right-handers, are language, calculation, and praxis. Bedside assessments include the following:
Language
Spontaneous speech
The analysis of spontaneous speech is a vital aspect of language assessment for the classification of aphasia. This should be done after listening to several minutes of spontaneous conversation and after asking the patient to describe a complex scene such as the one shown in Fig. 7.2 in Chapter 7. However, it should be noted that this analysis is much more readily applied to aphasia resulting from strokes and other focal lesions than to the aphasia seen in patients with degenerative brain disease. Deficits can be considered under the following headings:
Naming
The ability to name objects or pictures is impaired in virtually all aphasic patients, and is probably the best index of overall severity. A range of items of varying similarity should be used, since aphasics, in common with normal subjects, show a marked frequency effect. That is to say, they are much more likely to show errors when naming low-frequency (less familiar) objects. This can be assessed using everyday items and parts of objects. Watch and pen are high-frequency items; winder, buckle, and nib are low-frequency items. The type of error which occurs is also helpful diagnostically. Patients with anterior (Broca’s type) aphasia typically produce the initial sound of a word, and are helped by phonemic cueing. Conduction aphasias produce multiple phonemic errors (TELOP, TELE, TELEPHONT for TELEPHONE). Semantic paraphasias (for example, CLOCK for WATCH, APPLE for ORANGE) are frequent in Wernicke’s aphasia, sufferers from which may produce totally neologistic utterances. Semantic errors also characterize the anomia of Alzheimer’s disease. Patients with semantic dementia are typically very anomic and produce semantic errors and particularly broad subordinate responses (‘animal’, ‘musical thing’, etc.). It should be remembered that accurate identification of visually presented objects also depends upon intact perceptual processes; the occurrence of visually based naming errors and difficulty in visual identification in the absence of other language deficits should suggest a visual agnosia (see ‘Visual object agnosia’ in the ‘Damage to Specialized Right Hemisphere Functions’ section in Chapter 3). There are several easily administered formal tests of naming ability, including the Graded Naming Test and the Boston Naming Test (see Appendix). The ACE-III includes 12 line drawings: two easy items (watch and pencil) from the MMSE and 10 harder items (five animals and five objects).
Comprehension
It is common to overestimate the comprehension abilities of aphasic patients on the basis of their understanding of unstructured conversation. In free conversation there are gestural, facial, and prosodic (tone-of-voice) cues. Thus, fluent aphasics can often respond appropriately to opening conversational gambits (‘How are you today?’), despite profound comprehension problems. Body-part commands may also be very misleading; responses to axial commands such as ‘Close your eyes’, ‘Open your mouth’, and ‘Stand up’ are commonly preserved. The reason for this preservation is obscure.
Testing comprehension with difficult three-part commands (for example, ‘Touch your left ear with your right index finger and then touch my hand’) leads to erroneous underestimation of the comprehensional abilities, since these commands are not only grammatically complex, but also overload short-term (working) memory capacity, and require right–left understanding.
Comprehension is best tested by asking the patient to point first in response to single words and then in response to sentences of increasing complexity.
The most widely used formal test of language comprehension is the Token Test, in which the subject has to follow commands of increasing syntactic complexity. The Test for the Reception of Grammar (TROG) was developed to assess language development but is very useful in assessing adults with suspected syntactic disorders (see Appendix). The most frequently used aphasic test, the Boston Diagnostic Aphasia Examination, includes tests of word and sentence comprehension as does the Western Aphasia Battery developed in London, Ontario.
Repetition
Repetition should be tested with a series of words and sentences of increasing complexity. It is best to start with short single words, and then to progress to polysyllabic words and finally sentences. The sentences should include ones that are rich in small grammatical function-words, which are particularly difficult for aphasic patients. Patients can then be graded on their ability to repeat accurately. As mentioned previously, the contrast between repetition and comprehension is often very informative in separating patients with semantic dementia from those with progressive non-fluent aphasia (PNFA). The former have no difficulty repeating words such as ‘hippopotamus’, ‘eccentricity’, ‘unintelligible’, and ‘statistician’ (the words in the ACR-III) but have no idea of their meaning. By contrast, those with PNFA show the opposite profile: impaired repetition but good understanding. Phrases without meaning such as ‘no ifs, ands, or buts’ are usually more difficult than sentences like ‘The orchestra played and the audience applauded’. Striking impairment in sentence repetition is also characteristic of logopenic progressive aphasia.
Aphasics who cannot repeat have lesions involving the perisylvian language structures. Disproportionately severe breakdown of repetition is found in conduction aphasia and in patients with so-called speech apraxia who make gross phonetic errors with omissions, substitutions, and distortions when repeating. Lesions outside the primary language zone and progressive degenerative disorders spare repetition, producing what are termed transcortical aphasic syndromes (see ‘Transcortical aphasias’ in the ‘Language’ section in Chapter 3).
Reading
Both reading aloud and reading comprehension are important, but must be carefully distinguished. Failure to comprehend is usually accompanied by incorrect reading aloud. However, there are patients who cannot read aloud correctly, but have good understanding. If the patient successfully reads words and sentences, the capacity to read and understand a short paragraph should be tested. Simple reading comprehension can be tested by writing down a command such as ‘Close your eyes’ or ‘Place your hands on top of your head if you’re aged over sixty’. More complex comprehension can be assessed by asking the patient to read a paragraph from the newspaper and then asking questions about the content.
In most instances, reading skills parallel spoken language abilities. However, occasionally alexia may occur with agraphia, but without other aphasic deficits. Even more rarely, alexia may exist without even agraphia; this is called ‘pure alexia’ or ‘alexia without agraphia’.
Once a reading problem has been uncovered, the next step is to determine which aspects of the normal reading process have broken down. The various types of dyslexia have been described (see ‘Disorders of Reading: The Dyslexias’ in Chapter 3), and consist of the following:
Letter identification
Errors in single-letter reading and the strategy of laboriously naming each letter (letter-by-letter reading), sometimes aided by tracing the letter outline with the finger, are characteristic of pure alexia.
Types of reading errors
Reading a word as another conceptually related, but not sound-related, word (ACT for PLAY, SISTER for UNCLE, OCCASION for EVENT) is seen in deep dyslexia in which visual errors are also common (SHOCK for STOCK, CROWD for CROWN, etc.). Errors confined to the initial part of the word occur in neglect dyslexia (for example, FISH for DISH) secondary to right hemisphere damage.
Effects of word regularity
Selective difficulty in reading words that do not obey the normal soundto-print rules of English—so-called exception words—with a tendency to produce regularization errors (PINT to rhyme with MINT) is the defining characteristic of surface dyslexia. In the context of progressive neurodegenerative disorders, the finding of surface dyslexia points strongly to a diagnosis of semantic dementia.
Non-word reading
Patients with deep dyslexia, in which there is a breakdown in the sound-based reading route, are unable to read plausible non-words (NEG, GLEM, HINTH, DEAK, etc.). In deep dyslexia other deficits are present; but in phonological dyslexia the only major problem is with reading these nonsense words.
To screen for dyslexic syndromes, the list given in Table 5.4 contains non-words, regular words, and exception words of mixed frequency. The ACE-III contains an abbreviated list of six exception (irregular) words.
Writing
Writing ability can be analysed in terms of the manual execution of writing, recall of individual letters and words, and sentence composition. Three major types of dysgraphia are recognized (see ‘Disorders of Writing—The Dysgraphias’ in Chapter 1):
Table 5.4 A word-list for screening dyslexic syndromes
| Exception words | Regular words | Non-words | ||
|---|---|---|---|---|
| Pint | Soot | Shed | Board | Neg |
| Gauge | Steak | Nerve | Bridge | Glem |
| Sew | Suite | Wipe | Gaze | Gorth |
| Naïve | Aunt | Ranch | Flame | Mive |
| Thyme | Tomb | Swerve | Mug | Rint |
| Mauve | Height | Hoarse | Vale | Plat |
| Epitome | Dough | Sparse | Pleat | Hinth |
| Cellist | Sieve | Scribe | Ledge | Deak |
Spontaneous writing
It is usually sufficient to screen for dysgraphia by asking patients to compose a sentence about a subject of their choice. If they are unable to think of anything, suggest a recent journey or a description of their home. Defects in letter formation, spelling, and grammatical composition should be readily apparent. If errors occur, then analysis of the specific deficit is required.
Note: it is not adequate merely to sample a patient’s signature. Many severely dysgraphic patients maintain the ability to write their name, which can be thought of almost as an automatic reflex activity.
Writing to dictation
To analyse the type of linguistic deficit in writing it is useful to have a list that contains words with regular sound-to-spelling correspondence and words with exceptional spelling. The list suggested earlier for reading will also serve this purpose.
Oral spelling
If the disorder of writing appears to be motoric, in that individual letters are poorly formed, reversed, or illegible, then it is useful to check oral spelling, which is normal in dyspraxic and neglect agraphias.
Calculation
We do not routinely assess numerical and calculation abilities in our memory disorders clinic unless there is a suggestion of deficits in this domain on patient and/or carer enquiry or the patient is aphasic.
Number reading and writing
Number reading and writing should be assessed before arithmetic abilities by asking the patient to do the following:
Arithmetic operations
Only after number reading/writing has been assessed should the patient’s ability to understand arithmetic operations be assessed as follows:
Praxis
Tests of apraxia can be divided in the following way:
Virtually all aphasic patients are impaired on miming to command, but performance often improves when imitating the examiner. A common error is the use of ‘body-part-as-object’, so that, for instance, when miming the use of a toothbrush, the forefinger substitutes as a brush, or when showing how to use a pair of scissors, the patient uses the index and middle fingers. The majority of apraxia patients perform meaningless gestures very poorly, and are worse at gesturing to command compared to copying or using real objects. A schedule for examining buccofacial and limb gestures is shown in ‘Praxis’ in the ‘Additional Material for Particular Cases’ section in Chapter 7.
Right Hemisphere Functions
Functions associated with the (for right-handers) non-dominant right hemisphere are:
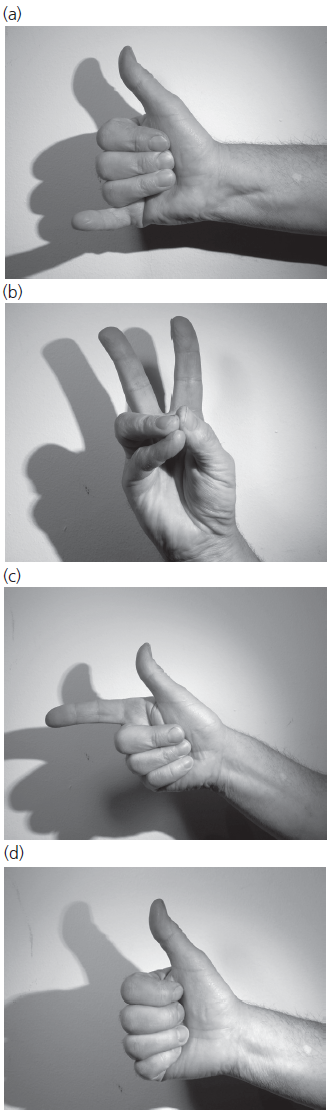
Fig. 5.2 A sequence of hand positions helpful in testing for apraxia.
Personal neglect
Many patients with acute left hemiplegia do not realize that they are paralysed, and some frankly deny their deficit even when specifically challenged. This type of deficit is overlooked because examiners take it for granted that hemiplegic patients are aware that they are paralysed down one side. To detect these disorders it is necessary to question all stroke patients about their deficits and to compare their subjective assessments with objective findings. The following hierarchy of denial phenomena can be applied:
Manifestations of personal (bodily) neglect
Personal neglect may be apparent because patients fail to groom one side of their head or shave one half of their face. Occasionally they have difficulty in dressing one side, or bump into objects on one side—usually the left. Head and eye deviation away from the neglected side (towards the lesion) implies damage to the frontal eye fields, and is a poor prognostic sign.
Sensory neglect
Patients with severe neglect may consistently ignore sensory inputs from the side contralateral to the side of their brain lesion. This usually occurs with right-sided lesions, so that the stimuli to the left are ignored. The following modalities should be tested.
Visual: the patient may ignore all visual stimuli to the contralateral side; if severe, this may be impossible to distinguish from hemianopia.
Auditory: the patient appears not to hear sounds to one side, and ignores visitors seated on that side of the bed.
Tactile: the patient ignores all sensory inputs from the affected side.
Sensory extinction to bilateral simultaneous stimulation is seen when the patient responds when stimuli (visual, auditory, or tactile) are presented to one side, but when simultaneously stimulated from both sides consistently ignores the neglected side.
Extrapersonal (hemispatial) neglect
Neglect of one half of space is fairly common after damage to either hemisphere; but persistent severe hemispatial neglect is seen only after right-sided damage. The following tests can be used to detect neglect phenomena.
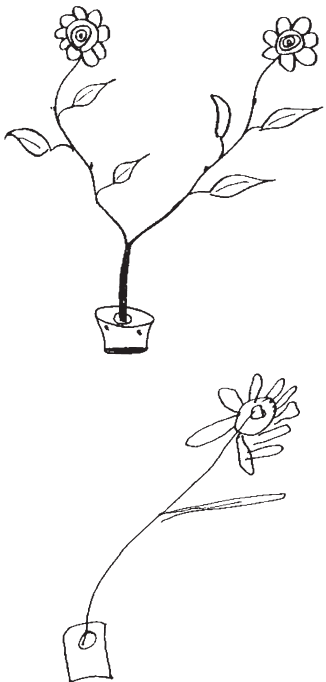
Fig. 5.3 Unilateral visual neglect: a right hemisphere stroke patient’s attempt at copying the double-headed daisy, showing classic neglect of the left side.
Provided by Dr Peter Halligan.
Neglect dyslexia and dysgraphia
These conditions are almost invariably associated with right-sided brain damage. Neglect dyslexia may affect lines of text or individual words. In the former, the patient omits the initial (left) part of each line, so that he or she reads only part of the text, rendering it nonsense. In the written equivalent, the patient writes on the right half of the page, and often leaves a progressively widening margin.

Fig. 5.4 Object-centred neglect: an example of a neglect patient’s copy of three items in a single array.
Provided by Dr Peter Halligan.
In word-based dyslexia, errors occur on reading the initial letters of words, which may be omissions (ISLAND to LAND) or substitutions (GRANT for PLANT). Word-based neglect dysgraphia causes the same type of errors, but in writing.
These syndromes are usually noted during language testing. But patients with other phenomena of neglect should be asked specifically to read a section of text from any book or magazine with wide columns. The word-list previously suggested for checking reading and writing should also detect word-based neglect dyslexia and dysgraphia.
Dressing apraxia
This is best detected by questioning family members or nursing staff. It may be observed on the ward. If there is any suggestion of dressing difficulty, a good test is to observe the patient putting on a shirt/blouse which has been turned inside out.
Visuospatial and constructional ability
Disorders of constructional ability are best detected by getting the patient to copy 3D drawings, such as a wire cube, or a complex 2D shape, such as the interlocking pentagons which form part of the Mini-Mental State Examination even patients with quite severe impairment of constructional skills may be able to copy simpler shapes, such as a Greek cross (Fig. 5.5).
For a more stringent and quantitative test, the Rey–Osterrieth Complex Figure Test is recommended, since the patient’s copy can be scored using standard criteria (Fig. 5.6). Delayed recall of the figure, usually after 30–40 minutes, can also be used as a measure of non-verbal memory.
Other formal tests for visuospatial and constructional abilities include the following:
Block design from the WAIS.
Benton Line Orientation Test.
Components of the Visual Object and Space Perception (VOSP) battery.
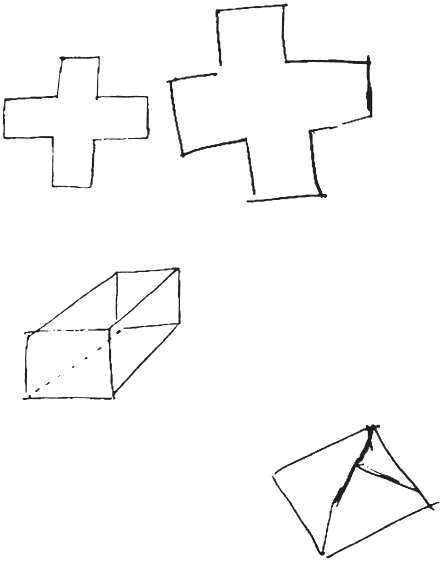
Fig. 5.5 Copy of a Greek cross and cube by a patient with a right-sided lesion, showing preservation of simple drawing but an inability to copy the 3D cube.
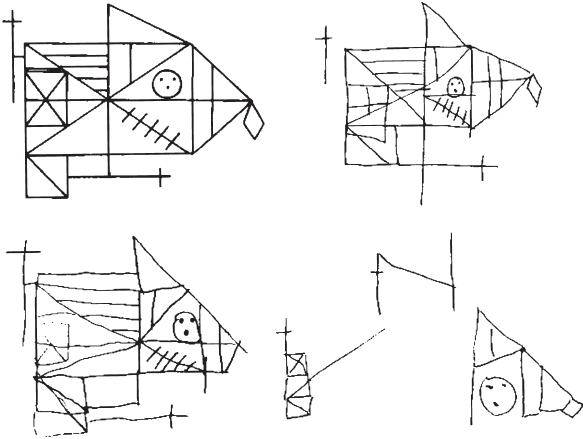
Fig. 5.6 The Rey–Osterrieth Complex Figure (upper left) and the copies of three patients with mild (upper right), moderate (lower left), and severe (lower right) impairment of constructional abilities.
Complex visuoperceptual abilities and the agnosias
Deficits in object and face recognition are difficult to assess at the bedside without special test materials; but if there are clues that some form of agnosia may be present the following relatively simple tasks can be employed:
Visual object agnosia
If the patient is unable to recognize simple objects or pictures despite good visual acuity and intact language abilities, a form of visual agnosia should be suspected.
In apperceptive visual agnosia, there is a breakdown at the stage of perceptual analysis, so that the patient is unable to describe the visually presented item and to match it with identical items. Patients’ copies of drawings will be slow and fragmented, and identification of real objects is better than that of photographs or of line drawings. Knowledge of the unidentified objects is preserved when tested verbally, and patients can identify objects by touch (see ‘Apperceptive visual agnosia’ in the ‘Damage to Specialized Right Hemisphere Functions’ section in Chapter 3).
In associative visual agnosia, the perceptual stages of object recognition are preserved, but patients are unable to make sense of the visual information; object description and matching are normal, and they can copy line drawings. In most cases, the deficit represents a loss of semantic knowledge (see ‘Associative visual agnosia’ in the ‘Damage to Specialized Right Hemisphere Functions’ section in Chapter 3). This causes an inability to name or identify items presented by any sensory modality, and a loss of verbal knowledge about the same items when asked probing questions (see Table 5.56).
Object feature description denotes the ability to describe the shape, outline, surface features, and colour of the presented object or picture.
Visual identification denotes the ability to recognize accurately the attributes of the visually presented stimulus even if unable to produce the name (for example, ‘It’s one of these things used by doctors to listen to your heart’).
Copying line drawings is tested by asking the patient to copy drawings of representational items such as a flower, a bicycle, a house, and so on.
Object matching denotes the ability to match identical objects or pictures of objects. To test this it is necessary to use an array of items or pictures, two of which are identical. The patient is asked to point to the two items that are the same.
Object knowledge means the ability to generate accurate verbal descriptions when given the name of objects which the patient cannot identify visually (‘What is a stethoscope?’ etc.).
Tactile naming is tested by getting the patient to name objects by palpation with the eyes closed.
Table 5.5 Differentiating the forms of visual agnosia
| Apperceptive | Associative | |
|---|---|---|
| Object feature description | × | ✓ |
| Visual identification | × | × |
| Copying line drawings | × | ✓ |
| Object matching | × | ✓ |
| Object knowledge (from name) | ✓ | × |
| Tactile naming | ✓ | × |
×, affected; ✓, spared.
Prosopagnosia
Patients with severe deficits in visual analysis causing apperceptive agnosia are invariably impaired at recognizing faces. The syndrome of prosopagnosia is a specific form of associative agnosia in which visual perception of faces, and hence the ability to describe and match faces, is preserved, but there is a disorder of face recognition and identification and is usually the result of a right posterior temporal lobe stroke. In suspected cases the following functions should be assessed:
There is another form of prosopagnosia in which knowledge of people is lost found in association with progressive atrophy of the right temporal lobe (a form of semantic dementia). Such patients lose the ability to recognize people but unlike classic post-stroke prosopagnosia they are unable to provide information from faces or names. Initially, the impairment affects less commonly encountered people such as stars or politicians from the past but as it progresses, loss of knowledge for more contemporary and common figures occurs.