Chapter 3
Localized Cognitive Functions
Introduction
The functions ascribed to the dominant, usually left, cerebral hemisphere show much more clear-cut laterality than those associated with the so-called minor hemisphere. This applies particularly to spoken language. Since language is such an important component of human cognition, and aphasia frequently complicates both focal and diffuse degenerative brain disease, I have dedicated a large section to discussing aspects of normal and abnormal language function. There then follows a brief description of disorders of calculation (acalculia) and of higher-order motor control (apraxia).
The second half of the chapter deals with disturbed right hemisphere functions: neglect phenomena, dressing and constructional apraxia, and complex visuoperceptual deficits (agnosias).
Localized cognitive functions can be summarized as follows:
Language
The general outline of this section is as follows:
Aphasia
Aphasia is defined as a loss or impairment of language function caused by brain damage. Language should be separated from speech, since the two may be damaged independently. Speech is the term applied to coordinated muscle activity for oral communication and to the neural control of this activity; language is the complex symbolic signal system used by individuals to communicate with one another. Clearly language is not only a spoken system, as communication occurs by reading and writing, and these functions may break down independently, to produce alexia or agraphia*, respectively. Language disorders may also be observed in the congenitally mute who use sign language.
Disturbances of articulatory processes arise from a variety of pathologies involving peripheral speech mechanisms, as in bulbar palsy, and in cerebellar and basal ganglia deficits. Dysarthria frequently accompanies acute anterior left hemisphere lesions, but may also occur with acute right-sided lesions. Thus dysarthria and aphasia may coexist, but one is often seen without the other. Mutism is a complete failure of speech output which, if acquired, usually signifies either a severe language disorder or an articulation disorder, although occasionally mutism may be seen in psychiatrically ill patients (catatonia or hysteria).
Causes of aphasia
Focal lesions
Dementias
Causes of mutism
Strokes
Disorder of articulation: language and writing normal
Psychiatric disorders
Cerebral dominance for language
The left hemisphere is strongly dominant for language functions in most humans. Therefore aphasia very rarely complicates right hemisphere damage in individuals who write with their right hand; when this does occur it is referred to as ‘crossed aphasia’. The functional dominance has anatomical parallels; the superior part of the temporal lobe, the planum temporale, is consistently larger on the left side. The situation in left-handers is more complicated; left hemisphere dominance in these individuals is commonly stated to be around 50–60%. In fact, most people who do not show a strong preference for writing with their right hand are, to some degree, ambidextrous. Commensurate with this, their language functions are more equally divided between the two hemispheres.
Applied anatomy
Within the left hemisphere, the area of supreme importance for language comprehension and production is the posterior superior temporal lobe (Wernicke’s area). Deficits in this area consistently produce gross problems with the decoding of spoken and written language, and in the assembly of correct language output with phonological and semantic speech errors. The other major language area is in the inferior frontal lobe (Broca’s area) and the adjacent anterior insula. Lesions here produce faltering, non-fluent, and distorted language output, with simplified or disturbed grammatical structure, although the comprehension of spoken and written language is largely intact. The insula is thought to be key for phonological assembly and lesions restricted to this area cause so-called speech apraxia in which patients have great difficulty repeating strings of syllables. The inferior frontal and superior temporal regions are connected by means of the arcuate fasciculus; lesions here classically cause conduction aphasia, although this syndrome most commonly results from damage to the supramarginal gyrus or surrounding areas (see Fig. 3.1).
One extremely important concept (based in the past on lesion and electrophysiological studies in patients with acquired pathology and, more recently, on functional activation by positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) in normal volunteers) is that Wernicke’s area acts as the ‘gateway’ between the amodal semantic or knowledge system and modality-specific language areas. Patients with lesions to Wernicke’s area do not lose knowledge about things in the world as evident from their ability to use objects appropriately and perform picture–picture matching tests. Put simply, they know what a fork or stethoscope is when given the item but have lost the ability to map the arbitrary phonemes ‘F’_ ‘ORK’ to that object. This contrasts with the cross-modal loss which occurs in patients with semantic dementia (see ‘Semantic dementia’ in the ‘Dementia’ section in Chapter 2).
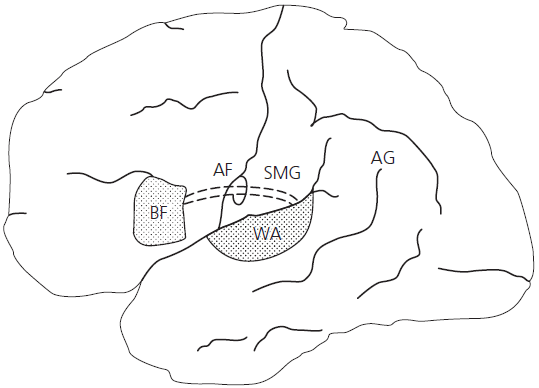
Fig. 3.1 Principal language areas. AF, arcuate fasciculus; AG, angular gyrus; BA, Broca’s area; SMG, supramarginal gyrus; WA, Wernicke’s area.
The area most associated with writing ability is the angular gyrus, which is the posterior extension of Wernicke’s area, and is situated at the junction of the temporal, parietal, and occipital lobes. Lesions that include the angular gyrus area cause Gerstmann’s syndrome, consisting of dysgraphia, dyscalculia, right–left disorientation, and a peculiar deficit in recognition of body parts called finger agnosia.
The minor hemisphere and language
The earlier-mentioned statements concerning language dominance require some qualification since not all aspects of language show such hemispheric specialization (see Table 3.1). It has become apparent from experimental studies of split-brain subjects (i.e. studies following corpus callosum section for intractable epilepsy) that, even in right-handers, the right hemisphere has a considerable capacity for understanding simple words, especially nouns, although it is unable to utilize the apparatus of speech for responding. This limited ability of the non-dominant hemisphere may explain some of the recovery seen even after devastating left hemisphere damage with resultant global aphasia. Also notable is the right hemisphere’s role in some non-linguistic aspects of language expression and comprehension. Although the linguistic components—phonology, syntax, and semantics—convey the principal meaning of language (see later in this chapter), there are in addition more subtle modulations which we use to imply attitude and emotion. These features have been termed prosody, which refers to the melody, pauses, intonation, stresses, and accents that enhance and enliven speech. Severely dysprosodic speech occurs with anterior left hemisphere damage. More subtle deficits in conveying and interpreting the emotion or affective components of language consistently accompany right-handed lesions—so-called emotional dysprosody. This is interesting in the context of other non-language-based specialization of the minor hemisphere. Patients with right hemisphere damage may show impairment on emotional judgement tasks involving faces.
Table 3.1 Definitions and neural bases of language functions
| Language function | Definition | Neural basis |
|---|---|---|
| Phonology | Production and comprehension of appropriately sequenced speech sounds (phonemes) | Left superior temporal lobe |
| Semantics | Assignment of meaning to words and production of linguistically appropriate individual words | Anterior and inferior temporal lobe (representations) and Wernicke’s area (mapping) |
| Syntax | Assembly of strings of words into sentences using pronouns, prepositions, tenses, etc. | Broca’s area and anterior insula cortex |
| Prosody |
(i)
Fine tuning by intonation, stress, cadence, etc.
|
Left anterior hemisphere, basal ganglia |
|
(ii)
Emotional expression
|
Right hemisphere |
Neurolinguistics made simple
True aphasia results from the breakdown in the linguistic components of language. These can be divided into phonological, semantic (or lexical), and syntactic aspects.
Phonology
This is the term applied to the sound pattern of human language. The smallest segment of spoken language is the phoneme, which is more or less the same as the sound represented by a single letter in alphabetic writing systems, such as the sounds represented by the letter ‘k’ in ‘kiss’ or the letters ‘sh’ in ‘should’. Each language consists of a finite number of phonemes, which can be ordered to produce an almost infinite number of words. They can therefore be considered the building blocks of language. Patients may be impaired in the ability to organize phonemes in sequence, which results in phonemic (or literal) paraphasias, which may be real-word approximations (SITTER for SISTER, STALE for SNAIL, etc.) or neologisms (FENCIL for PENCIL, POOT for SUIT, BORINGE for ORANGE, etc.). Phonological decoding (necessary for distinguishing PEAR from BEAR, or FIT from BIT) is clearly critical for language comprehension. Both phoneme production and decoding depend on the superior temporal region. Most patients with middle cerebral artery strokes and aphasia have some degree of impairment in phonological processing. Phonological speech errors also occur in logopenic progressive aphasia which is a specific manifestation of Alzheimer’s disease.
A closely related element of speech production is motor planning. Breakdown in this function, known as apraxia of speech, produces distortions of speech which are not transpositions of whole phones but rather random distortions affecting longer or complex words with hesitations and groping for sounds producing a loss of the normal melody (prosody) of speech. If severe, speech sounds slow deliberate and robotic in quality. Apraxia of speech occurs in people with Broca’s aphasia and is also characteristic of progressive non-fluent aphasia.
Semantics
The term semantics denotes the referential meaning of words. The fact that we know the correct meanings of ‘aunt’, ‘uncle’, ‘sister’, and so on, and that ‘canary’ refers to a small yellow bird, depends on our ability to map this arbitrary sound pattern into the underlying conceptual representation. This process can break down in two ways: a problem with the mapping process (as in Wernicke’s aphasia) or a loss of the representation (as in semantic dementia). Our store of words is sometimes called the ‘mental lexicon’, but semantics refers to more than a simple store of word forms—it encompasses our fund of knowledge of the world. This is discussed more fully in the section on semantic memory (see main ‘Memory’ section in Chapter 1). Breakdown within the semantic system results in a failure to understand the referential meaning of words, so that on naming or in spontaneous speech, paraphasias (ORANGE for APPLE, SISTER for BROTHER, etc.) or superordinate substitutions (ANIMAL for GIRAFFE) are produced. Mere failure to access the correct word in the lexicon typically produces word-finding difficulty, with abrupt cut-offs in speech or circumlocutions (‘it’s that thin green vegetable that you eat with your fingers’ (asparagus)). Comprehension clearly depends on the accurate assignment of meaning to heard words. A breakdown in this process impairs single-word comprehension. The dominant temporal lobe plays a key role in lexico-semantic processes. Neuroimaging studies indicate that the superior temporal region (Wernicke’s area), the basal temporal areas (areas 20 and 35) and the angular gyrus (area 37) form a complex network, with Wernicke’s area being the central coordinating region.
Syntax
Words are strung together to form phrases or sentences in a complex way that obeys strict grammatical rules. The correct use of these non-substantive components of language—articles, prepositions, pronouns, adverbs, verb endings, and so on—is referred to as syntax. A reduction or loss of syntactic production, agrammatism, is found in patients with Broca’s type aphasia. The production of sentences with incorrect use of these syntactic elements, termed paragrammatism, is a feature of Wernicke’s aphasia. Disorders of comprehension affecting predominately the syntactic aspects of language can also be demonstrated in patients with damage to the inferior frontal lobe and in the dementias.
Each of these components of language—phonology, syntax, and semantics— can be independently damaged. Furthermore, the deficit may involve input, output, or both. Since the neural circuits underlying these processes function in parallel and overlap anatomically, focal lesions invariably produce complex deficits. Many neurolinguists would argue that no two aphasia patients are exactly alike; but, luckily for clinicians, recognizable clinical syndromes usually emerge, at least after the phase of acute damage. It is worth emphasizing the point that the classical descriptions of the aphasic syndromes (Broca’s, Wernicke’s, and conduction aphasia, etc.) were based on chronic stable brain lesions. It is often difficult to apply this classification to acute stroke patients, the majority of whom have either a global aphasia or an atypical unclassifiable aphasia. Similarly, patients with language breakdown secondary to progressive degenerative brain disease, such as Alzheimer’s or frontotemporal dementia, do not develop classical aphasic syndromes. For these reasons, analysis of language disturbance is best considered in terms of the linguistic components outlined previously.
Theories of reading and writing
A similar linguistic analysis can be applied to disorders of reading and writing. In the case of writing, phonology becomes orthography (or spelling). In this respect, it is important to remember that the rules of English orthography are complex, with many unique exceptions. By knowing the rules of English pronunciation, it is possible to read and spell many words correctly (HINT, GLINT; GAVE, BRAVE; CASE, BASE; etc.) and plausible non-words (NEG, GLEM, GORTH, etc.); but not words with irregular spelling-to-sound correspondence (for instance, PINT; HAVE; ISLAND; YACHT). Clearly such irregular or exceptional words cannot be read or spelt correctly by applying spelling-to-sound rules, but rather must be pronounced or spelt by directly accessing word-specific knowledge about their phonology and orthography. The evidence from patients with acquired dyslexia has been used to argue that there are two parallel systems for reading and writing: one utilizes a sound-based route for reading and writing, and the other uses the more direct meaning route (see Fig. 3.2). These systems can break down independently, to produce different types of dyslexia and dysgraphia, which are described later in this chapter. An alternative view is based upon computational interactive models of cognition. The so-called triangle model proposes that three core processes—semantics, phonology, and orthography—interact (Fig. 3.3). This system quickly learns to read correctly regular words based on print-to-sound correspondences in the language without the need for semantic support. Irregular words present more difficulty (as anyone with children learning to read and spell English knows) and the system has to learn each of these unique word-to-sound mappings. Some irregular words have very frequent occurrence in English (HAVE, ONCE) and are quickly learnt, others are of low frequency (MAUVE, GIST, EPITOME) and are learnt slowly, if ever. For the latter words, semantic support is very important because when semantics break down, patients have difficulty pronouncing and spelling low-frequency irregular words (this is termed ‘surface dyslexia’).
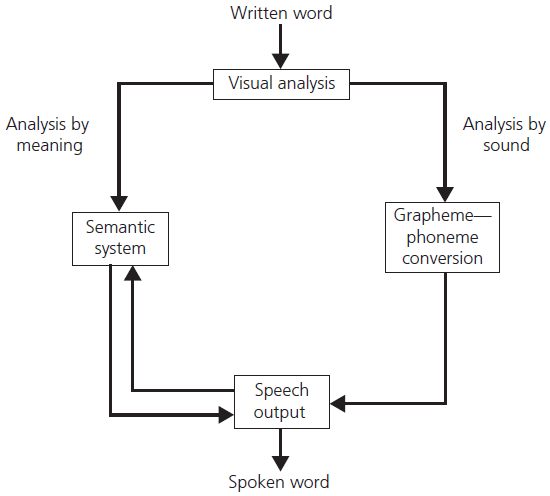
Fig. 3.2 Dual-route model of reading.
Classifying aphasia syndromes
I have avoided the terms expressive and receptive aphasia, which, in my opinion, are misleading; virtually all aphasic patients have difficulty with language expression, although the linguistic processes underlying the deficit differ. Patients with left anterior lesions have a disturbance of language output, producing laborious and distorted speech. Posterior lesions produce a fluent language output, with phonemic and semantic paraphasic errors. Both patient groups have problems with ‘expression’.
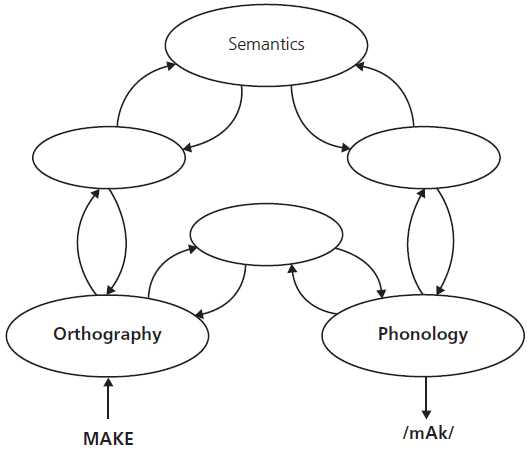
Fig. 3.3 Triangle model based on computational theories.
For the purpose of gross clinical diagnosis and clinico-anatomical correlation, four aspects of language should be considered (see Table 3.2).
Table 3.2 Classification of aphasic syndromes according to four parameters
| Type of aphasia | Fluency | Repetition | Comprehension | Naming |
|---|---|---|---|---|
| Global | Non-fluent | × | × | × |
| Broca’s | Non-fluent | × | ✓ | × |
| Transcortical motor | Non-fluent | ✓ | ✓ | × |
| Wernicke’s | Fluent | × | × | × |
| Transcortical sensory | Fluent | ✓ | ✓ | × |
| Conduction | Fluent | × | ✓ | × |
| Anomic | Fluent | ✓ | ✓ | × |
×, affected; ✓, relatively spared.
Common aphasic syndromes: Broca’s, Wernicke’s Conduction, Transcortical, and Anomic
For each of the more common aphasic syndromes, I shall describe the nature of the spontaneous speech, performance on tests of naming, repetition, and comprehension, writing and reading, and the anatomical localization.
Broca’s aphasia
In the fully developed syndrome, speech output has two principal characteristics—it is non-fluent and agrammatic—although these two features can dissociate. Typically, there is impairment of word initiation and phoneme selection. This results in slow, effortful, and laboured speech, which is distorted with frequent word approximations which may be phonological or, more commonly, due to a degree of apraxia of speech. Attempts at word or sentence repetition show the same features. The second major component of spontaneous speech is agrammatism. This is a simplification of grammatical form, with a notable reduction in function words (prepositions, articles, etc.). At its most severe, the patient is restricted to telegraphic utterances. It should be noted that this feature is present only in a minority of cases; most patients with Broca’s aphasia manifest only a simplification or reduction in syntactic complexity rather than an absolute loss.
Naming on confrontation is impaired, but the patient often responds when a phonemic cue (the beginning sound of the word) is provided, and is able to choose the correct name from among a number of alternatives. Auditory comprehension, although typically preserved in ordinary conversation, may break down when it is studied by using syntactically complex commands (‘touch the book after touching the pen’). The written output of patients with Broca’s aphasia mirrors their spoken language. It is characterized by mis-spellings, letter omissions, perseverations, and agrammatic sentences. Reading aloud is disturbed. On single-word reading, the syndrome of deep dyslexia (see ‘Deep dyslexia’ later in this chapter) may occur, in which subjects make frequent semantic errors (SISTER for UNCLE, PARROT for CANARY, etc.), and are unable to read small function words, or unfamiliar, phonologically plausible non-words (CHOG, LAVE, GORTH).
Anatomical localization The term ‘Broca’s aphasia’ has become more descriptive than anatomical. Neuroimaging studies have shown that lesions purely restricted to Broca’s area (the inferior frontal lobe) produce a transient disturbance in speech output, not the other features of Broca’s aphasia. The symptom complex of Broca’s aphasia occurs after more extensive damage to the frontoparietal region, corresponding to the area supplied by the anterior branch of the middle cerebral artery. Moreover, the fully developed syndrome is rarely encountered in acute stroke patients, but evolves over time from a more global aphasic syndrome. When speech apraxia is prominent, then this suggests damage to the anterior insula. In such patients there is disintegration of speech output and they have inordinate difficulty repeating multisyllabic words (e.g. caterpillar) and sequences of syllables (PA … TA … KA) leading to multiple approximation attempts. As noted earlier, patients with progressive non-fluent aphasia also have features of speech apraxia.
Wernicke’s aphasia
In Wernicke’s aphasia, spontaneous speech is fluent and paraphasic. In the acute stages, speech output often consists of strings of phonological and semantic paraphasias and their combinations, sometimes producing neologistic jargon. In contrast to Broca’s aphasia, there is little effort in speaking, and no dysarthria. Indeed, in many cases there is an increased speech production rate, with a tendency to acceleration. Melody and intonation are preserved. It would therefore be impossible to detect Wernicke’s aphasia in a patient speaking a language unfamiliar to the examiner. There is relative preservation of grammatical structure, but speech lacks information-conveying nouns and verbs (‘Yes, I should say so’, ‘I mean’, ‘I’m a redax’, ‘No toxicat’, ‘That is to say …’, ‘You know what I mean’, etc.). Often abnormal syntactic inflections are produced; this is termed paragrammatism. Patients are usually unaware of their communication problem. Naming is severely impaired; patients often produce phonological or semantic errors, but are not aided by phonemic cues, and are typically unable to select the correct name when offered a choice by the examiner.
Auditory comprehension is always impaired. In severe cases, patients are unable to point on command to common objects in an array (for example, ‘point to the keys’); but simple body commands may be preserved. Linguistically, patients have difficulty with phoneme discrimination, and with assigning mapping strings of phonemes to their internal semantic representation.
The comprehension of written text is usually similar to auditory comprehension. However, some patients have superior reading ability, perhaps in association with relative sparing of more anteriorly placed parts of the superior temporal lobe. When writing, letters are well formed, but patients produce aphasic, disjointed, and repetitive text, containing few nouns and verbs.
Anatomical localization Unlike Broca’s aphasia, Wernicke’s aphasia correlates fairly well with destruction of Wernicke’s area. Right-handed patients with the full-blown syndrome of fluent, paraphasic, and paragrammatic speech and severe impairment of auditory comprehension almost invariably have suffered damage to the posterior superior temporal lobe of the left cerebral hemisphere. The extent of the comprehension deficit and the prognosis for recovery depends on the degree of damage to Wernicke’s area.
Conduction aphasia
Named after damage to the main conducting tract (arcuate fasciculus) joining Broca’s and Wernicke’s areas, conduction aphasia is characterized by fluent but paraphasic speech. The paraphasias are mainly phonological (for example, SITTER for SISTER, FENCIL for PENCIL). In contrast to Wernicke’s aphasia, comprehension of speech and written material is much better. Repetition is highly abnormal; patients typically produce strings of phonemic approximations in an attempt to repeat a phrase, termed conduit d’approche (ROY ARTCRY … ROYIT ARTIL … ROYOT ARTIMERY, etc.). Digit span is characteristically very limited. There is almost always anomia with phonological errors. Reading aloud parallels the performance of repetition; but comprehension of silent reading may be very good. This pattern of impairment is also seen in patients with so-called logopenic progressive aphasia.
Anatomical localization The traditional locus of pathology in conduction aphasia has been in the supramarginal gyrus, that is, the gyrus lying above and around the posterior end of the Sylvian fissure and the adjacent white matter tracts (see Fig. 3.1) which thereby separates the temporal from the frontal language areas. Many exceptions to this classic localization have been reported, although most cases have involved lesions round the Sylvian fissure. Conduction aphasia most often occurs at a stage of recovery from Wernicke’s aphasia. When it occurs as an acute syndrome the prognosis for complete recovery is very good.
Transcortical aphasias
Early aphasiologists observed that some patients with aphasia retained competence at repeating language which they did not understand. They postulated the existence of a ‘transcortical pathway’ directly linking the ‘auditory language centre’ and the ‘verbal motor centre’, thus bypassing meaning. The term ‘transcortical’ has persisted, despite abandonment of the supporting theory, and is now used purely descriptively.
The features common to the transcortical dysphasias are preserved repetition and cortical or deep white matter damage at, or beyond, the periphery of the perisylvian language areas.
Transcortical motor aphasia Transcortical motor aphasia (TMA) shares many similarities with Broca’s aphasia: spontaneous language output is very sparse and dysarthric, but with few paraphasic errors. Sentence repetition is, by contrast, strikingly preserved, and comprehension of verbal and written language is very good. Written output parallels spoken output. Lesions responsible for TMA are located in the dominant frontal lobe anterior and superior to Broca’s area. This is the type of aphasia typically seen with anterior cerebral artery infarction, and may follow a period of initial muteness. In these cases the critical lesion is in the supplementary motor area in the superomedial parasagittal region of the frontal lobe. TMA may also occur in patients with frontotemporal lobar degeneration (see ‘Frontotemporal dementia’ in the ‘Dementia’ section in Chapter 2).
Transcortical sensory aphasia Transcortical sensory aphasia (TSA) is similar to Wernicke’s aphasia, the language output being fluent but contaminated with semantic paraphasic errors. Comprehension is severely defective at the level of linking sound to meaning. However, phonemic processing is intact, and the patient is therefore able to repeat words and long sentences, but cannot extract meaning from language. Reading and writing are similar to those in Wernicke’s aphasia. The site of the lesion is said to be in the border zone of the temporoparietal junction, which therefore preserves the primary language areas, but disconnects them from posterior brain areas. A language syndrome akin to TSA occurs in advanced Alzheimer’s disease and in patients with the temporal lobe variant of frontotemporal lobar degeneration, better known as semantic dementia. In the latter syndrome the fluent aphasia is simply one manifestation of a more generalized or amodal loss of knowledge (see ‘Semantic dementia’ in the ‘Dementia’ section in Chapter 1).
Anomic aphasia
Difficulty in word-finding on confrontational naming tasks is the rule in virtually all aphasic patients. Problems with word access in free conversation producing either abrupt cut-offs in mid-sentence, circumlocutions, or paraphasic substitutions, are also ubiquitous. Only when the severity of naming problems stands out above all other language deficits is the term ‘anomic aphasia’ used. This is a common syndrome. It is a frequent residual deficit following recovery from one of the other types of aphasia, and is the characteristic language abnormality in the earlier stages of Alzheimer’s disease. A space-occupying lesion present anywhere in the dominant hemisphere may manifest as anomic aphasia.
Anomia is, therefore, the least useful localizing sign in aphasia. But the acute onset of pure anomic aphasia suggests a lesion in the left temporoparietal area. When the injury extends to the angular gyrus, alexia and agraphia may appear.
Category-specific anomia This is the term given to a deficit in naming items of a particular category. A well-documented form of this is colour anomia. Patients have a specific deficit in naming colours on confrontation or in pointing to colours when they are named by others (see ‘Achromatopsia, Colour Agnosia, and Colour Anomia’ later in this chapter). Other examples of category-specific anomias involve naming living things or non-living things. In the latter syndromes there is loss of general knowledge about the affected category, so that generating definitions, answering questions about semantic features, and comprehending on picture-pointing tests are also impaired. Since these deficits affect more than purely naming, they are more properly considered as disorders of semantic memory (see ‘Semantic memory’ in the ‘Memory’ section in Chapter 1). Patients who have sustained temporal lobe damage from herpes simplex virus encephalitis seem to be particularly vulnerable to category-specific semantic memory deficits.
It is worth noting at this point that the process of naming, although apparently simple and automatic in normal circumstances, depends upon a complex sequence of processes—visuoperceptual, semantic, lexical, phonological, and articulatory—each of which may be disrupted. Disorders of visuoperceptual and semantic processing are considered more fully under the heading of ‘Visual object agnosia’ later in this chapter.
Formal tests of language
Disorders of Reading: The Dyslexias
Disturbances of reading can be divided into two broad categories: (i) those in which there is a defect in the early visual components of decoding written script, the so-called peripheral dyslexias; and (ii) those in which there is a breakdown in the normal linguistic processes involved in deriving meaning from words, the central dyslexias (see Table 3.3).
Peripheral dyslexias
Alexia without agraphia (pure alexia)
This rare syndrome was important in establishing the concept of internal disconnection of cortical areas although the theoretical interpretation of pure alexia is now more controversial. In most cases, there is an acute inability to comprehend any written material. By contrast, the patient recognizes words spelled aloud. Writing is preserved, but patients are unable to read their own written output. Spoken language is also normal. With time, the ability to read individual letters often returns. When this happens, words are spelled aloud by the patients and recognized auditorily, so that they adopt a ‘letter-by-letter’ reading strategy. Because of this, there is a marked word-length effect, so that, unlike unaffected people, patients with letter-by-letter reading are very slow at reading longer words. The syndrome is usually accompanied by right homonymous hemianopia. Defects in colour naming (with intact colour vision) or impairment of colour perception (achromatopsia) may also occur (see ‘Achromatopsia, Colour Agnosia, and Colour Anomia’ later in this chapter). This symptom complex usually accompanies infarction of the medial aspect of the left occipital lobe, often with involvement of the splenium of the corpus callosum, following occlusion of the left posterior cerebral artery (see Fig. 3.4). The classic theory for the genesis of alexia without agraphia is as follows: because of the right hemianopia, patients cannot read in the right visual field. Words can be seen on the left side, and are therefore projected to the right hemisphere. However, the lesion in the splenium prevents transfer of the visual information from the right to the left side. The primary language areas are spared, but are disconnected from incoming visual information. The strategy adopted of identifying each individual letter is thought to occur initially in the right hemisphere, which then enables access to pronunciation in the left hemisphere. More recently this disconnection has been doubted, rather it has been argued that the infarction damages the so-called word form area which disrupts the ability to process whole words but also single letters to be decoded.
Table 3.3 Types of dyslexia and their localizations
| Types of dyslexia | Localization |
|---|---|
| Peripheral dyslexias | |
| Preserved oral and written spelling, and ability to identify words spelt aloud | |
|
Left medial occipital lobe |
|
Right hemisphere lesions |
| Central linguistic dyslexias | |
| Linguistically based, invariably affect oral spelling | |
|
Left temporoparietal region and semantic dementia |
|
Extensive left hemisphere lesions |
|

Fig. 3.4 Alexia without agraphia: lesion causes interruption of information flow to the left-sided language areas from ipsilateral and contralateral visual areas (via splenium).
Neglect dyslexia
In neglect dyslexia, which usually complicates right parietal lesions, there is failure to read correctly the left half of words (for example, LAND is read for ISLAND, PEACH is read as BEACH, etc.). This syndrome is discussed more fully in the context of other hemineglect phenomena (see ‘Neglect phenomena’ later in this chapter). Neglect dyslexia arising from a left hemisphere lesion and thereby affecting the right half of words is exceptionally rare and difficult to detect.
Central (linguistic) dyslexias
Most aphasic patients have some disturbance of either reading aloud or of comprehension of text. Indeed, this is one of the most sensitive markers of language disturbance, and many patients who have otherwise recovered from acute aphasic syndromes find that they no longer derive pleasure from reading. In the aphasic syndromes, reading aloud usually parallels other oral language abilities. Broca’s aphasics have particular difficulty reading grammatical morphemes (function words like OF and AT, and verb inflections such as -ED) and make numerous errors, producing laboured and faltering oral reading. Their comprehension of complex text is usually poor. Most patients with moderate or severe Wernicke’s aphasia are severely dyslexic, and make numerous paraphasic errors. Reading is relatively intact in patients with diffuse brain damage and in the early stages of Alzheimer’s disease. Since the ability to pronounce irregular words correctly is highly educationally dependent, a test of irregular word reading, the National Adult Reading Test (NART), is widely used to predict premorbid intellectual ability. Two broad types of linguistically based dyslexic syndrome can be distinguished on single-word reading.
Surface dyslexia
In this form of dyslexia, there is breakdown in the whole-word (lexical) representations, so that reliance is placed on sub-word correspondences between letters and sounds (the so-called grapheme–phoneme conversion system). This use of the ‘surface’ features produces few problems reading words with regular sound-to-spelling correspondence. But errors occur when attempting to read words which deviate from the typical pattern of spelling-to-sound correspondence in English, so-called exception words (PINT, ISLAND, MAUVE, etc.). The most frequent mistake is to produce regularization error (PINT to rhyme with MINT). There is usually a marked frequency effect, so that the ability to read low-frequency irregular words is most affected. As well as occurring with posteriorly placed left temporoparietal strokes, this syndrome is almost universal in semantic dementia and in other patients with breakdown in the semantic system. The theory advanced to explain surface dyslexia is described earlier in this chapter (see ‘Theories of reading and writing’).
Deep dyslexia
This extremely rare syndrome is characterized by an inability to translate orthography to phonology, which means that patients with this disorder are required to read entirely via meaning. They are completely unable to read plausible non-words such as NEG, GLEM, and GORTH. The cardinal symptom which is likely to bring attention to deep dyslexia is the semantic error: when trying to read single words aloud, the patient produces responses related in meaning (but not sound) to the target (for example, reading CANARY as PARROT, TULIP as CROCUS, SISTER as UNCLE, etc.). Visual errors are also common (for example, SWORD for WORDS, SCANDAL for SANDALS). There is usually great difficulty in reading small function words (IS, OF, AND, THE, etc.), and a relative impairment in reading abstract compared with concrete words. Most patients with deep dyslexia have suffered extensive left hemisphere damage. Opinions are divided as to whether the features of deep dyslexia result from the residual malfunctioning left hemisphere, or from the right hemisphere’s attempt at reading. The latter gains support from the characteristics of right hemisphere reading in split-brain patients, which resemble in many ways the features of deep dyslexia.
Phonological dyslexia
Phonological dyslexia is a rare form of dyslexia that affects mainly the ability to read non-words.
Tests of reading ability
See Chapter 5 for details.
Disorders of Writing: The Dysgraphias
The production of well-formed and linguistically correct, flowing script depends upon the integration of motor control, visuospatial and kinaesthetic functions, and the symbolic aspects of the language system. It is not surprising, therefore, that writing abilities are fragile, and that brain dysfunction of very varied types produces dysgraphia. Dysgraphia is more prominent than dyslexia in patients with degenerative brain disease. It is a striking early feature in corticobasal degeneration. Three main varieties of writing disturbance can be identified (see Table 3.4).
Dyspraxic dysgraphia
Writing disturbance is said to have a dyspraxic quality if there is a disturbance in the smooth automatic production of written elements due to a breakdown in motor control. Letters may be inverted or reversed, and are often illegible. Copying is also abnormal. Oral spelling is preserved. Dyspraxic dysgraphia most often accompanies dominant parietal lobe damage, and features of ideomotor limb dyspraxia are usually present. Dominant frontal lobe lesions may occasionally produce pure dyspraxic dysgraphia.
Spatial or neglect dysgraphia
This disorder of writing usually accompanies non-dominant hemisphere lesions. It can be easily differentiated from the other dysgraphias because of the invariable association with other visuospatial and perceptual abnormalities (spatial neglect, drawing problems, etc.), and by the characteristics of the writing: a wide left margin and a tendency to miss out, or mis-spell, the first few letters of individual words (RUSH for BRUSH, DOY for JOY, etc.).
Table 3.4 Types of dysgraphia and their localizations
| Types of dysgraphia | Localization |
|---|---|
| Dyspraxic dysgraphia | |
| Oral spelling intact, defective copying | Dominant parietal or frontal lobe |
| Neglect dysgraphia | |
| Wide left margin or mis-spelling of initial part of words. other neglect phenomena present | Right hemisphere lesions |
| Central (linguistic) dysgraphias | |
| Written oral spelling affected | |
|
Left temporoparietal region and semantic dementia |
|
Extensive left hemisphere damage |
|
Unknown |
Central (linguistic) dysgraphias
These almost always accompany some degree of spoken language disturbance or dyslexia. The pattern of deficit tends to parallel the accompanying aphasia. Anteriorly placed dominant hemisphere lesions produce slow, effortful writing which is poorly formed, with mis-spellings, omissions, reversals, and perseverations. Agrammatism may also be observed. Patients with Wernicke’s aphasia may have preserved motor aspects of handwriting ability, but produce paraphasic errors and show word-finding impairments. Difficulty spelling and writing is a common early feature of corticobasal degeneration.
In parallel with the central dyslexias, two broad types of linguistic dysgraphia can be distinguished.
Lexical (surface) dysgraphia
The lexical (semantic) system uses whole-word retrieval by consulting internal memory stores of known spellings. This system is important for spelling familiar but orthographically irregular words (for example, CHOIR, PINT, ISLAND, NAIVE) and homophones (words with the same pronunciation but different spelling, for example, ATE–EIGHT). Damage to this system produces a lexical agraphia characterized by particular problems in spelling irregular words and the production of errors that are phonologically plausible (MENIS for MENACE, COFF for COUGH, etc.). This syndrome has been described in patients with lesions in rather diverse sites in the left temporoparietal region. It is also a fairly consistent finding in patients with advanced Alzheimer’s disease and with semantic dementia in whom there is a breakdown of the semantic system (see ‘Semantic dementia’ in the ‘Dementia’ section in Chapter 2).
Deep dysgraphia
The alternative, phonological, spelling system uses sound–letter (phoneme– grapheme) rules. Disruption of this system produces phonological agraphia, in which patients are unable to spell unfamiliar words and non-words (for example, VIB, CHOG, LAVE).
Deep dysgraphia results from more profound breakdown in the sound-based spelling route, with additional damage to the semantic system. As in deep dyslexia, semantic errors occur (SISTER for AUNT, SKY for SUN), and there is a strong effect of word class, in that those affected are better at spelling concrete than abstract words. Most patients with this syndrome have suffered extensive left hemisphere damage.
Phonological dysgraphia
In the majority of patients with linguistically based dysgraphias, oral spelling and written spelling are equally impaired. As a general rule, disturbed writing with spared oral spelling suggests a dyspraxic or neglect dysgraphia.
Tests of writing ability
Syndromes of Calculating Impairment
Acalculia, anarithmetria, and spatial dyscalculia
Acalculia, a disturbance in the ability to comprehend or write numbers properly, is common in patients with aphasia; but rare instances where number and language abilities dissociate have been reported. The angular gyrus region in the left hemisphere appears to be important for numeracy. A separate disorder, anarithmetria, is characterized by the inability to perform number manipulations. Patients with this disorder correctly recognize and reproduce individual numbers and know their values, but cannot perform computations (addition, subtraction, etc.). This disorder is relatively common in patients with dementias, particularly Alzheimer’s disease. A third cause of difficulty performing written calculations is so-called spatial dyscalculia. This syndrome, in which patients have difficulty aligning columns of figures and performing carrying tasks, complicates right hemisphere damage, and is invariably associated with other neglect phenomena.
Gerstmann’s syndrome
This rare symptom complex is also referred to as the angular gyrus syndrome, because of the localization of the causative lesions. The features are:
Since these features can occur in isolation or in any combination, the usefulness of this syndrome in clinical practice is rather questionable.
Disorders of Praxis: The Apraxias
Apraxia is the inability to carry out complex motor acts despite intact motor and sensory systems and coordination, good comprehension, and full cooperation. The term ‘apraxia’ should be applied only to deficits with a motoric basis. Several unrelated disorders use the same term (dressing apraxia, construction apraxia, verbal apraxia of speech), but really deserve more accurate titles, and will not be considered in this section. Four main types of motor apraxia are recognized (see Table 3.5).
Limb kinetic apraxia
Patients with this form of apraxia have a breakdown of fine motor organization and the coordination of finger movements necessary to perform fine motor tasks. They are particularly poor at copying meaningless hand positions and better when mimicking meaningful gestures (saluting, waving, etc.) and typically use real objects flawlessly. This pattern is observed in patients with basal ganglia and supplementary motor area (SMA) pathology. It is characteristic and prominent in the early stages of corticobasal degeneration although other forms of apraxia are seen as the disease progresses.
Ideomotor apraxia
This disorder mainly accompanies aphasia but can be seen without a frank language disorder. Patients are unable to carry out motor acts to command, but typically perform the same acts spontaneously. There is difficulty with the selection, sequencing, spatial orientation, and movements involved in meaningless and meaningful gestures (waving, beckoning, etc.), and in demonstrating the use of imagined household items (for example, a toothbrush or comb) or tools. Imitation improves performance and patients are considerably better when using real objects.
In right-handed patients, ideomotor apraxia is associated with left hemisphere lesions. The critical areas are the inferior parietal and prefrontal areas. Such lesions may either destroy motor engrams (cortically stored movement patterns) or disconnect the flow of information necessary for initiating complex motor acts. Anterior callosal lesions can cause the inability of one limb—usually the left—to perform on command, even though the other limb performs normally.
Table 3.5 Types of apraxia and their localizations
| Types of apraxia | Localization |
|---|---|
| 1. Limb kinetic | Basal ganglia, supplementary motor area (SMA) |
| 2. Ideomotor | Left parietal lobe |
| 3. Ideational or conceptual | Left temporal lobe |
| 4. Orobuccal (oral) | Left inferior frontal lobe |
Ideational or conceptual apraxia
The term ideational apraxia has been applied to the inability to carry out a complex sequence of coordinated movements, such as filling and lighting a pipe or making a cup of tea, although, in contrast to what happens in ideomotor apraxia, each separate component of the sequence can be successfully performed. This seems to be a very rare disorder and might relate more to frontal dysfunction. It has also been used to describe the inability to mime the use of objects (for example, a toothbrush) and, importantly, to use the actual object due to a loss of the underlying conceptual knowledge. Therefore a better term is conceptual apraxia. The issue of whether knowledge of object use constitutes a separable domain of semantic memory has been a topic of controversy. There are reports of patients with apparently isolated conceptual apraxia, although evidence from semantic dementia suggests a common integrated semantic system. This form of apraxia is seen in patients with semantic dementia and in advanced Alzheimer’s disease. In the latter group, it is difficult to unravel the contribution of apraxia from the confounding effects of poor language comprehension and diminished attention.
Orobuccal (oral) apraxia
Patients with oral apraxia have difficulty performing learned, skilled movements of their face, lips, tongue, cheeks, larynx, and pharynx on command. For example, when they are asked to pretend to blow out a match, suck a straw, or blow a kiss, they make incorrect movements. The critical areas for lesions causing this deficit are the inferior frontal region and the insula. Thus oral apraxia commonly accompanies Broca’s aphasia. Some of the speech-output deficits in Broca’s aphasia may result from apraxia of speech (i.e. difficulty with articulation and phonation secondary to impaired motor programming). Orobuccal apraxia is also seen in patients with frontotemporal dementia, progressive nonfluent aphasia, and corticobasal degeneration.
Damage to Specialized Right Hemisphere Functions
Deficits related to right hemisphere damage (in right-handed individuals) are much more difficult to detect than those caused by comparable dominant hemisphere damage. Often the deficits are subtle, and have not been noticed by the patient or observers (see Table 3.6). Thus it is arguably more important to assess any patient with suspected cognitive impairment carefully for these deficits, since aphasia and apraxia will usually be readily apparent.
It should also be noted that all of the functions described in this section are only relatively lateralized to the right hemisphere: spatial and visuoperceptual skills are both bilaterally represented, but the hemisphere that is non-dominant for language is more specialized with aspect to these abilities. The deficits described in this section are more severe and long-lasting with right hemisphere damage, but virtually all of them can be found to lesser degrees with left-sided lesions.
Table 3.6 Deficits arising from right hemisphere damage
|
|
| Personal: |
Denial of hemiplegia (anosognosia) Unconcern over deficit (anosodiaphoria) Neglect of grooming, shaving, etc. |
| Motor and sensory: |
Hypokinesia Visual, auditory, and tactile neglect Sensory extinction to simultaneous bilateral stimulation |
| Extrapersonal: |
Hemispatial neglect (e.g. drawings, line bisection, visual search) Neglect dyslexia and dysgraphia |
|
|
|
|
|
Object recognition (apperceptive and associative agnosia, optic aphasia) |
|
Prosopagnosia |
|
Achromatopsia, colour agnosia, and anomia |
|
|
|
|
|
|
|
* nb: these functions are not very well lateralized, but deficits are more common and more severe with right hemisphere damage.
Neglect phenomena
There is substantial evidence that the right hemisphere in man is more important than the left for spatially directed attention. The term ‘attention’ is applied rather broadly in neuropsychology to a number of different phenomena. I have used the qualifier ‘spatially directed’ to separate this form of attention directed to personal and extrapersonal space from the more general meaning of attention in the context of concentration/attention, which was discussed in Chapter 1. Deficits in spatially directed attention produce unilateral neglect.
The term ‘neglect’ has been used to describe a complex of behavioural abnormalities. At its most profound, there is neglect of attention to both personal and extrapersonal space although these two phenomena are separable.
Personal neglect
In its most extreme form, patients behave as if one half—usually the left—of their body has ceased to exist. If hemiplegic, they deny any impairment, a phenomenon termed anosognosia. They may even deny the existence of half their body, claiming that their left arm is someone else’s. More frequently, patients admit that they have a neurological deficit, but appear unconcerned about it. This has been termed anosodiaphoria. Initially patients with neglect may ignore stimuli presented to the side contralateral to their lesion, whether the stimulus is visual, tactile, or auditory. Later, they become able to detect these stimuli, but when given simultaneous bilateral stimulation will fail to report the stimuli presented to the contralateral side. This phenomenon is called extinction to double simultaneous stimulation. It is most often observed in the visual and tactile modalities. Patients with severe personal neglect shave, groom, and dress only their right side, and even only eat the food on the right half of the plate. Failure to move their head and eyes to the side opposite to the lesion and motor akinesia of the contralateral limb may also be observed.
Motor and sensory neglect
Motor or intentional neglect involves a response failure that cannot be explained by weakness, sensory loss, or inattention. There may be failure to move a limb (limb akinesia) or the limb can be moved but only after a long delay and strong encouragement (hypokinesia). Patients with intentional neglect who can move may make movements of decreased amplitude. They may also have an inability to maintain postural movements, known as impersistence. Patients with motor neglect, who can move their contralesional limb, may fail to move this limb (or have a delay) when they are required to move their ipsilateral limb. Limb akinesia, hypokinesia, hypometria, and motor impersistence can affect some or all parts of the body including the limbs, eyes, or head. Patients with motor neglect may also have intentional biases such that there is a tendency to move towards the ipsilesional space.
The same type of phenomenon is seen in the sensory realm. Sensory neglect involves the selective defect of a deficit in awareness, which may apply to all stimuli on the affected side of space, or may be confined to stimuli impinging on the patient’s body (personal neglect). The modalities affected by neglect may vary: subtypes of sensory neglect exist for the visual, auditory, and tactile modalities. The deficit in awareness is accompanied by an abnormal attentional bias. Once attention is engaged on the ipsilesional side, subjects may have difficulty disengaging their attention and moving to the contralateral side. If the lack of awareness and attentional bias are present only when there is a competing stimulus at the ipsilesional location, the disorder is known as extinction. Many patients with sensory neglect recover and become able to detect isolated contralesional stimuli but continue to manifest extinction most typically in the visual or tactile realm.
Extrapersonal neglect
This is usually tested by asking patients to bisect lines of varying length, to perform cancellation tasks, or to draw and copy pictures. When asked to copy a drawing of an object such as a clock or house, patients typically fail to draw the left side. On line bisection tasks they place the half-way mark to the right of the mid-point which is particularly apparent using long lines. Tests involving the cancellation of letters or stars among other stimuli distributed across a page are particularly sensitive methods of detecting neglect. When writing, they may leave a wide margin on the left or occasionally omit the initial part of the word (neglect dysgraphia). On reading, there may be omission of the beginning of the line or even the initial letters of a word (neglect dyslexia).
In milder cases there is often no external manifestation of neglect, and only through specific testing by drawing and cancellation tests will the impairment be detected.
Applied anatomy and causes of neglect
Neglect is very common in the acute stages following damage to either the right or left cerebral hemisphere, but it is usually short-lived. Severe persistent unilateral neglect is found most often following damage to the right inferior parietal lobe (Brodmann areas 29 and 30) and, to a lesser extent, after right dorsolateral prefrontal cortex damage. Homologous areas in the monkey receive inputs from the higher-order sensory association cortex, the thalamic nuclei, and parts of the limbic system (especially the cingulate cortex). Outputs go primarily to the frontal eye fields, the striatum, and the superior colliculus. Thus the inferior parietal lobule can be considered as a centre for integrating sensory experiences, motivational responses, and visual search mechanisms. Although apparently widely distributed, these diverse brain areas (parietal, prefrontal and cingulate cortices, thalamus, and reticular system) are all intimately linked by reciprocal connections. Lesions of any one of these disrupt the mechanisms of spatially directed attention, and may therefore produce neglect phenomena. Acute frontal lobe injury usually results in ipsilateral head and eye deviation, accompanied by visual and personal neglect phenomena. Lesions of the thalamus, the basal ganglia, or the cingulate gyrus may also cause unilateral neglect. Neglect is most commonly observed in the context of strokes but is also found in association with tumours and occasionally in patients with neurodegenerative diseases.
Mechanisms of neglect
Many patients with unilateral extrapersonal neglect have accompanying hemianopia, and it is tempting to attribute neglect to the visual loss. However, neglect may also be seen in patients with intact visual fields, and many patients with complete hemianopia are able to orientate and follow into their blind half-field, and furthermore do not show neglect phenomena on drawing or cancellation tasks.
Attentional model
One popular model proposed to explain the occurrence of neglect after right hemisphere lesions is as follows. Whereas the left hemisphere contains mechanisms which maintain attention to the contralateral (right) half of the sensory world, the right hemisphere contains the neural apparatus for attending to both sides of space. Thus lesions of the left hemisphere produce no substantial deficit, since the intact right hemisphere can take over the task of attending to the right side. Right hemisphere damage, on the other hand, will cause left unilateral neglect, since the intact hemisphere lacks the mechanisms for ipsilateral attention (see Fig. 3.5). To explain the phenomena of personal neglect, it has been proposed that the parietal lobe contains representations of the body with these same asymmetries. An elaborated version of the attentional model proposes that spatial attention is composed of three elementary processes: engaging, disengaging, and shifting. Patients with right parietal damage are thought to have selective deficits in disengaging attention from stimuli to the right, resulting in an inability to shift and engage stimuli to the left. Recent work has also emphasized the deficit in spatial working memory found in neglect subjects: on cancellation tasks they are unable to keep track of which targets have been visited before, leading them to repeatedly go over and over the same spatial location.
Representational model
In a famous experiment carried out in Milan, patients with neglect were asked to describe the cathedral square as if standing on the cathedral steps overlooking the square. They accurately described the features on the right side of the square, but omitted the details on the left. They were then asked to imagine that they were standing at the opposite end of the square, facing the cathedral. Now, they described all the features to their right (which had previously been omitted) and neglected those to their left (which had previously been included). This neglect of internal imagery has subsequently been reported in many neglect patients, and can be tested at the bedside by asking patients to imagine that they are walking down a very familiar street and to describe all the buildings they would pass. Representational theories propose that the inability to form an adequate contralateral representation underlies the clinical phenomena of neglect. It is postulated that the right hemisphere is responsible for constructing a central map of space which is a direct analogue of sensory experience.
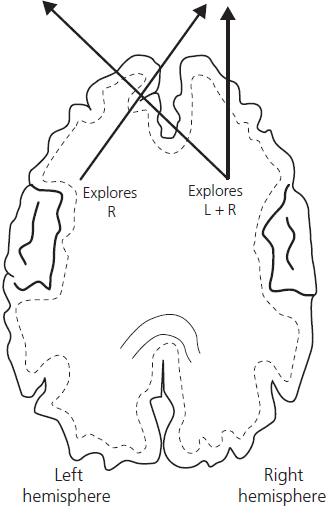
Fig. 3.5 A model of hemisphere specialization in directed attention in which only a right-sided lesion will lead to unilateral visual neglect.
At present, there is no entirely satisfactory unitary hypothesis to explain the diverse phenomena observed in neglect patients. It is probable that both attentional and representational models are, in part, correct.
Tests for unilateral neglect
See Chapter 5 and the Appendix for details.
Dressing apraxia
A disturbance in the ability to dress is fairly common following focal right hemisphere damage and more diffuse brain injury. The term ‘apraxia’ is inappropriate, since it is not a motor disorder. Instead, the deficit is in the orientation of body parts in relation to garments because of faulty visuospatial mechanisms. When there is a focal lesion, it is usually in the right posterior parietal area. Other phenomena of right hemisphere damage are invariably present. Patients with more advanced dementia or acute confusional states (delirium) may show the same problem.
Constructional disorders
Impairment in the ability to copy a visually presented model by drawing or assembling blocks has been termed constructional apraxia. As with dressing apraxia, this bears little relation to motor disorders.
To copy adequately a two-dimensional shape, such as a cube or star, requires normal visual acuity, the ability to analyse and perceive the elements of a drawing, and, finally, coordinated visuomotor ability. Given the complex nature of the task, it is not surprising that deficits can arise with right- or left-sided cerebral damage. However, constructional apraxia is more common, and more severe, in patients with lesions of the right hemisphere, especially if the parietal lobe is involved. There are also qualitative differences. Left-sided lesions lead to over-simplification in copying. Right-sided cases make gross alterations in the spatial arrangement, with so-called explosion of the constituent parts. Constitutional deficits are seen in patients with Alzheimer’s disease, particularly the visual variant, and are severe in patients with corticobasal degeneration.
Tests of constructional ability
See Chapter 5 and Appendix for details.
Complex visuoperceptual abilities
Although both hemispheres are involved in the processes of visual analysis, there is evidence for right hemisphere specialization. Patients with right-sided lesions have more substantial deficits on a range of visuoperceptual tasks, including:
A battery of standardized tests for the detection of abnormalities of this type, the Visual Object and Space Perception Battery (VOSP, see Appendix) is available, but is not suited to routine bedside use.
Subtle deficits in perceptual processing are impossible to detect at the bedside; but severe disorders of visuoperceptual processing may result in various forms of visual agnosia, which should be recognizable clinically.
Visual object agnosia
The term ‘agnosia’ can be roughly translated as ‘non-recognition’. Visual agnosia implies a disorder of recognition that cannot be attributed to general intellectual impairment, aphasia, or basic sensory dysfunction. A patient with visual object agnosia sees objects, but fails to recognize what they are. Agnosias may be visual, tactile, or auditory. Within a particular modality, agnosia can occur for different classes of stimuli such as colours, objects, or faces. Often patients are agnosic for more than one class of items, and sometimes in more than one modality. Since visual object and face agnosia are most common, I have concentrated on these.
There are two principal types of object recognition disorder: one involves the earlier perceptual stage of object analysis; in the other there is a breakdown in the processes by which meaning is ascribed to visual percepts (see Fig. 3.6). These disorders have been termed ‘apperceptive’ and ‘associative agnosia’, after the work of Lissauer in the late nineteenth century (see Table 3.7).
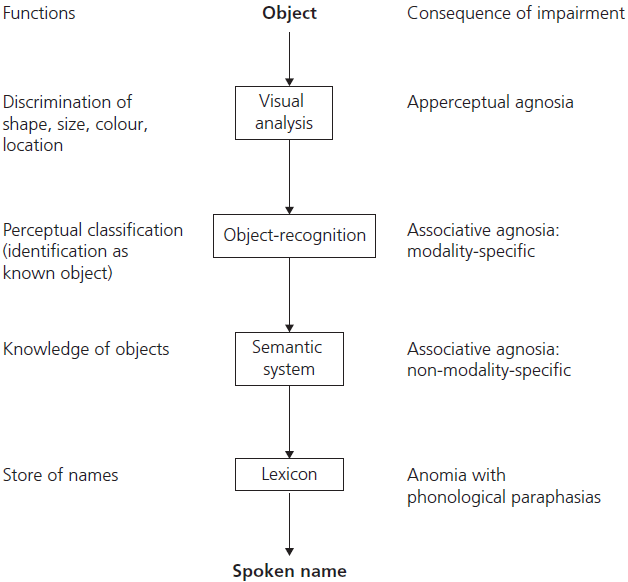
Fig. 3.6 A cognitive model of object recognition, understanding, and naming.
Apperceptive visual agnosia
Patients with this form of visual agnosia show preserved elementary visual faculties, such as acuity, simple shape and contour discrimination, and colour perception, but fail on more complex tasks involving object identification and naming. They are typically unable to copy shapes, or to discriminate two examples of the same object in arrays.
Visual fields may be normal; but most patients have defects on perimetry ranging from left hemianopia to marked tunnel vision. Despite being unable to identify visually presented objects, patients retain full knowledge about the unidentified items, and can name them by palpation or if given a verbal description. For instance, if shown a watch, patients with apperceptive agnosia would be unable to identify it as such, but if allowed to hold it would name it correctly. If asked to name the item ‘worn on the wrist and used to tell the time’ they would have no difficulty retrieving the word ‘watch’. The lesion in apperceptive visual agnosia usually involves fairly widespread bilateral posterior occipitoparietal regions. Interestingly, carbon monoxide poisoning appears to have a particular aetiological role. Cases with bilateral posterior watershed strokes, penetrating head injury, and mercury poisoning have also been described.
Table 3.7 The differentiating features of apperceptive agnosia and associative agnosia*
| Basic visual processing | High-level perceptual analysis | Naming and identification | Semantic knowledge | |
|---|---|---|---|---|
| Apperceptive agnosia | ✓ | × | × | ✓ |
| Associative agnosia | ✓ | ✓ | × | ×/✓ |
* In some cases semantic knowledge is preserved, whereas others show a pervasive disorder of object knowledge.
×, impaired; ✓, preserved.
Associative visual agnosia
This term has been applied rather loosely to patients with the inability to recognize visually presented objects despite apparently normal high-level perceptual processing. In classic cases the deficit is confined to the visual modality, while in others the deficit is more pervasive and multimodal (in more modern terminology the latter is referred to as a loss of semantic knowledge). The specific disorder of optic aphasia (see following ‘Optic aphasia’ section) is also sometimes included in this category.
Classic (modality-specific) associative agnosia
This is extremely rare. Patients have difficulty identifying or naming visually presented objects. Preservation of high-level perceptual processing can be demonstrated by their normal drawings of objects they cannot recognize, and by their ability to match pairs of such stimuli as the same or different. The traditional interpretation of this deficit considers the functional lesion to be one of accessing stored semantic knowledge from the visual modality, as a result of a disconnection in the flow of information (see Fig. 3.6). More recently it has been shown that high-level perceptual processes may not be entirely normal— patients are consistently better at recognizing real objects than photographs or line drawings, and the naming errors are invariably visual in nature. The site of pathology in such patients is variable: all have posterior quadrant damage, and in many it is bilateral; but cases with left unilateral posterior temporoparietal lesions have also been documented.
Cross-modal associative agnosia
In most cases of associative agnosia there is a generalized semantic memory impairment. The defect in object recognition is, therefore, not limited to visual presentation. These patients demonstrate an inability to identify objects in any modality (for instance, touch, or verbal description), as well as a loss of verbal knowledge which affects fine-grained (attributional) rather than broad category information. That is, they will be able to identify a picture as an animal, but unable to specify the type of animal. Likewise, on multiple-choice questions they will identify the word ‘tiger’ as the name of an animal, but make mistakes when asked about its size, habitat, ferocity, and so forth. A number of patients have been described in whom the loss of semantic knowledge is ‘category specific’, for instance, affecting living but not man-made things, or vice versa. Such deficits are considered more fully in the section on semantic memory (see main ‘Memory’ section in Chapter 1).
The locus of damage in patients with deficits in semantic memory invariably includes the left anterior temporal lobe. A degree of global semantic memory loss, resulting in features of associative agnosia, is present in patients with moderately advanced Alzheimer’s disease, and to a more marked extent in patients with semantic dementia (see ‘Semantic dementia’ in the ‘Dementia’ section in Chapter 1). Interestingly, in patients with ‘category specific’ loss of knowledge about living things the cause is very often herpes simplex virus encephalitis.
Optic aphasia
In this very rare syndrome, described by Freund in 1889, there is a disorder when naming or verbally describing visually presented items. In contrast to what is found in visual agnosia, patients with optic aphasia can recognize items visually, as demonstrated by their accurate pantomiming of their use, even though they cannot access their names. The deficit is modality specific, in that naming by tactile presentation and naming to description (for example, what do you call ‘a large triangular musical instrument with many strings played by plucking?’) are intact. Various explanations have been advanced to explain this strange syndrome. One influential account postulates a disconnection between stores of visual and verbal semantic knowledge. Thus object presentation activates intact visual knowledge, but verbal semantics cannot be assessed via this route; whereas, when one is given a verbal description, there is no difficulty with name access. Most cases are associated with right-sided visual field defects, achromatopsia, and/or alexia, since the site of damage is usually the left medial occipital region.
Tests for the detection and classification of visual object agnosias
See Chapter 5 for details.
The Cambridge semantic memory battery consists of a range of tasks based upon the same core set of 64 items (half natural and half man-made) with subtests designed to test input to and output from semantic knowledge about these items (see Appendix).
Prosopagnosia
This term describes the inability to recognize familiar faces. While patients state that all faces are unfamiliar or unrecognizable, they are able to use cues such as voice, gait, or distinctive clothing to identify familiar people.
Following contemporary models of cognitive processing, face identification proceeds from a perceptual to a recognition stage, whereby faces are categorized as familiar, and then compared with stored representations of known faces before the appropriate name can be produced (see Fig. 3.7).
In prosopagnosia, the deficit is at the categorization stage of this process since these patients are able to describe and identify facial components (for example, beard or nose), match faces in arrays containing examples of the same and different faces, and identify emotional expressions. In many cases they even retain the ability to perform complex visual matching tasks requiring the matching of faces taken under different lighting conditions and from different angles, although such tasks are usually performed slowly and laboriously. They also retain their knowledge of people they are unable to recognize, so that they may be unable to recognize a photograph of Margaret Thatcher, but when given the name can produce appropriate factual information. Not surprisingly, prosopagnosics are invariably impaired at learning new faces.
The question of how selective the deficit is to face processing is controversial; most, if not all, cases have problems with fine-grained identification such as types of flower, breeds of dog, and makes of car, leading some authorities to speculate that prosopagnosia is a defect in distinguishing items within categories containing many confusable exemplars.
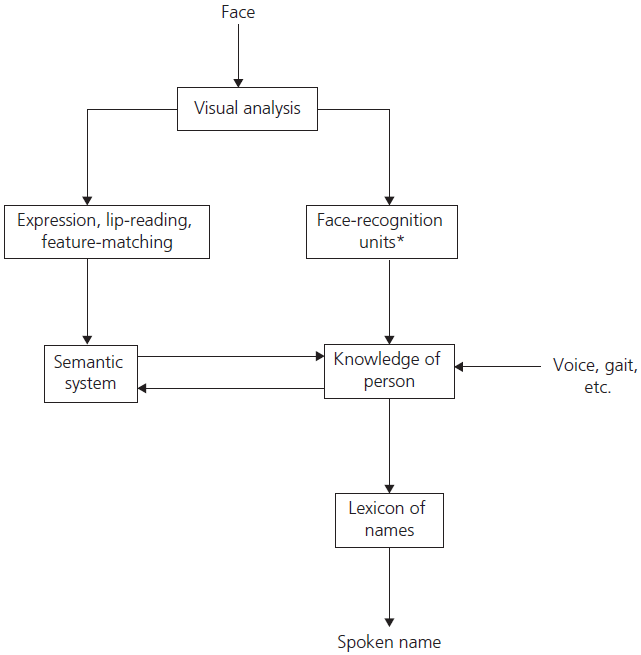
Fig. 3.7 A cognitive model of face recognition. FACE-Recognition units function as a memory store of known faces. A lesion at this level (*) causes prosopagnosia.
Prosopagnosia is most commonly associated with bilateral inferior occipitotemporal lesions, but occasional cases with purely right-sided lesions have been reported. Field defects are usually present, and many patients have additional deficits such as achromatopsia or pure alexia.
A variant of prosopagnosia occurs in the context of anterior right temporal lobe atrophy which is a homologue of semantic dementia. Patients complain of progressive difficulty with face recognition or naming, or both. Unlike post-stroke prosopagnosia the deficit is cross-modal. That is to say, they have difficulty identifying the people from their face and in producing information in response to the name (they are unable to name a photograph of Ronald Reagan, would not be able to name ‘the President of the USA who was an ex-actor’ and produce little, or no, information in response to the name). Another difference is that the deficit is dependent on the degree of familiarity: family, friends, and extremely famous people are still recognized, at least in the early stages.
Tests of face processing
See Chapter 5 for details.
Achromatopsia, Colour Agnosia, and Colour Anomia
Achromatopsia is an acquired disorder of colour perception characterized by a loss of ability to discriminate between colours. It may occur in isolation from other defects in object or form perception. It is usually symptomatic; patients complain that everything appears washed out, or ‘like black-and-white TV’. It may affect part or the whole of the visual field. The critical site of pathology is the medial occipitotemporal region. Pure alexia (alexia without agraphia, see ‘Alexia without agraphia (pure alexia)’ in the ‘Disorders of Reading: The Dyslexias’ section) and achromatopsia in the right hemifield often occur together after left posterior cerebral artery territory infarction.
In contrast, patients with colour agnosia are able to perceive and distinguish between colours, but are impaired on tasks requiring the retrieval of colour information (for example, ‘What colour is a banana?’). A specific disorder in colour naming with preservation of colour perception and of colour knowledge has also been reported under the heading of colour anomia. The latter syndrome may also be associated with alexia and right hemianopia, and is attributed to a disconnection of the left hemisphere language centre from visual information.
Tests of colour processing
Balint’s syndrome
This classic syndrome has three components: (i) psychic paralysis of gaze, that is to say an inability to direct voluntary eye movements to visual targets; (ii) optic ataxia, the inability to reach for, or point to, visual targets, also referred to as visual disorientation; and (iii) a visual attentional deficit in which only one stimulus at a time is apparently perceived, and even the attended stimulus may spontaneously slip from attention; this last feature is termed ‘simultanagnosia’.
Patients complain of severe visual difficulties, and may appear to be functionally blind. When faced with arrays of items or complex pictures they appear to be able to attend to only one small area at a time, with a resultant inability to synthesize the parts into a whole. Despite this severe limitation in what they can see at one time, visual fields may be full when they are challenged with gross stimuli. Patients exhibit a severe deficit in representing the relative location of objects relative to themselves, referred to as egocentric disorientation. More recent studies of patients with this pattern of deficits show consistent topographical disorientation, although this was not part of the original description. There are marked difficulties with spatial navigation.
The brain damage responsible is always bilateral, and includes the superior parieto-occipital region, damage to which interrupts the flow of spatial information from primary visual to parietal association areas. Cerebrovascular disease and prolonged hypotension leading to watershed infarction are the usual causes, although bilateral tumours and white matter disorders such as progressive multifocal leucoencephalopathy and mitochondrial disorders may also result in the same syndrome. In an outpatient setting, the commonest cause is so-called posterior cortical atrophy, a variant of Alzheimer’s disease (see ‘Atypical Alzheimer’s disease’ in the ‘Dementia’ section in Chapter 2).
Topographical disorientation
Considerable progress has been made in understanding the complex ability to navigate in previously familiar environments and to learn new routes quickly and without conscious effort. A loss of way-finding ability is known as topographical disorientation (see Table 3.8). The non-dominant parietal lobe, posterior cingulate, lingual, and parahippocampal cortices all contribute and can be considered a topographical network.
There is a crucial distinction between, on the one hand knowing and learning the spatial relationships between objects and landmarks in the environment versus, on the other hand, problems in the recognition of familiar landmarks. As with amnesia, another important dimension is the difference between anterograde impairment (i.e. the ability to learn a new environment) versus problems recalling the spatial layout of previously known environments.
Table 3.8 Topographical disorientation
| Egocentric disorientation | Inability to represent the location of objects relative to self. Co- occurs with features of Balint’s syndrome | Bilateral posterior parietal |
| Landmark agnosia | Inability to recognize salient environmental stimuli (buildings etc.) a form of associative agnosia | Lingual gyrus (basal occipital) |
| Anterograde spatial disorientation | Inability to create new maps or representations of the environment | Right parahippocampal gyrus (parahippocampal place area, PPA) |
Lesions to the posterior parietal cortex (typically bilateral) cause great difficulty in representing the location of objects relative to self, known as egocentric disorientation. This is typically associated with components of Balint’s syndrome and is extremely disabling. A variant of this syndrome affecting the ability to judge the position from which photographs of familiar buildings or objects are taken has been described in association with right posterior cerebral artery infarcts.
The ability to acquire new internal maps of an environment depends upon the posterior parahippocampal gyrus, a region known as the parahippocampal place area (PPA). Patients with lesions to the right PPA are completely unable to learn new routes and appear unable to encode information about novel spatial relationships. In contrast to these problems with spatial relationships and spatial route learning, patients with basal temporal lesions involving the lingual gyrus may develop a form of agnosia analogous to prosopagnosia but involving the recognition of previously familiar buildings.
* The terms aphasia and dysphasia are used interchangeably, although technically aphasia should mean loss of language function and dysphasia should refer to a disturbance of language. The same applies to the terms alexia and dyslexia, and to the terms agraphia and dysgraphia.